First of all, I updated the publication list below the last post regarding rare illnesses and CIPO. Another inpatient stay for pain management, so why not talk about pain?
The Pain's Reign (?) What I see in the mirror For now too long Pale, exhausted face Is it still me? Life has changed. Something so invisible Has such an influence Has it made me invisible, too? Drained, weak, poor. Detached from my older self, Detached from my newer body. Still never so aware of every cell in my body. Begging, needing, for life. Please, make it go away! That curse I don't wish on anybody Away from my fragile body! Can suffering be wrong when suffering is life? When pain takes away life Feeling of intensity and indifference, of life Feeling my body and yet not myself. Deep darkness I never knew existed Uncomfortability, pain, agony, suffering And so much more, inexplicable, indescribable What a misery – Isolated and alone with my companion Pain I cannot share, Wouldn't ever want to share Impossible to face alone. Constantly evolving, Endless hours of constant pain Sudden emergencies, or yet another flare? Inevitable, unfortunate. Monotonous days in the clinics Failed management plans Ups and downs of Incurable pain. When pain takes over Longing for its end Wandering in circles Waiting endlessly, patiently. Help! Travelling through my body, Into my mind. Through every single cell, through every single thought. When pain is so consuming, That I no longer exist But unite into one with my biggest enemy. Or should it rather be my best friend? Longing for the good old days Active, no worries, problems I would dream of now Running outside and full of energy How to regain strength and light? I want to open the window And take a deep breath of fresher air. How can I accept that it is closed? How can I cure those deep wounds? ‘Hope you are well soon, Hope the pain goes away quickly’ (...) Understanding is so low, Fellow sufferers, their loved ones do. Slow progression, fast decline, Faster progression, irreversible decline. Starving inside situations away from humanity Realisation. Acceptation. Chaos everywhere. Inside and outside. Pure Pain. Am I cursed? Am I an astronaut without a tank? Then at a point where Solution is survival only Tears of pain, tears of life It remains a silent cry for the end of pain. Scars that don't fade A prison in my body Stagnation Daydreaming of an impossible escape. Appreciate. How much more can I take? The next day I will have received the answer. Questions never stop. Insecurities. Pain unsettles the body and mind. A bird with broken wings Tired of fighting Tired of pretending Am I slipping away? Cannot pay attention or focus On anything else than this. Cherish little things. Be mindful. Value the beauty around. Difficult to realise. Am I fading away? Incomparable Feeling so heavy on me I am so heavy myself, A burden for those around me And so much burden to take Remember I am human only. Suffering so close and so afar, from my heart Suffering seeing my loved ones suffer as I suffer. Waiting for a cure. Waiting for improvement. Waiting for stabilisation. Waiting for the end of complications. Waiting for answers. Waiting for options. Waiting for ? Waiting in bed, waiting in clinics, waiting in full waiting rooms, waiting in grey places, waiting in everlasting pain. Deep breaths. When the pain steels actions, words and thoughts, Ratio, simple communication impossible Burned out and frustrated Interruptions of life. A never ending cycle just like the pain itself. Old ambitions fly so easily away, With a poor prognosis And life and hope slowly dies. Will I finally break (down) today? Can I please just float away? In silence. I have fought so hard. Incurable From its roots A human body of magic Turns into poor fragility. Pain is now, tomorrow? Infinite and woven in, all around me, within me Unavoidable. Unpredictable, uncertain, but Pain is mine Pain teaches me. Pain conveys my existence. No safe harbour. I am the harbour. I am safe. Gratitude. Longing for recovery Longing for relief. Still my pain So it is still me. Awareness. Throbbing, burning, stinging, cramping, shooting Flashs, bursts, spikes Dull, deep, stabbing, sharp, ripping Scary, agony, cruel, tiring, intensity 10/10 Twisting, curling up Like a knife, dagger, electric shoots, tearing me up Spot, spreading Flare ups, waves, constant cramps, flames Hot or cold Heavy Screams, cries, tears, Crying in pain. Smiling in pain. Where would we be without suffering? Do we actually need to suffer? Isn’t it a simple choice? It makes us grow, it teaches us, We endure and develop, receive so much compassion That we can spread It teaches us who we are and why we are alive. It is nature. Tranquillity.

If you want to continue reading, here are some more poems and recommendations.
Poems about physical suffering and/or illness:
- Pain has an element of blank, E. Dickinson
- On Pain, K. Gibran
- Being Visited by a Friend during Illness, Po Chu-i
- Sonnet 132, W. Shakespeare
- In the Fields Between Us, M. M. Brown
- Hymn to Physical Pain, R. Kipling
- For Suffering, John O’Donoghue
- Everything is Going to be All Right, D. Mahon
- Works by D. Hall and J. Kenyon e.g. The Ship Pounding
- Your Voice In The Chemo Room, M. Ritvo
- Pain: Composed in Sickness, S. T. Coleridge
- The Flower, G. Herbert
If you have any further recommendations about ‘physical pain poems’, please let me know.
More literature about pain and suffering (and finding purpose in it):
- All’s Well (fiction), M. Awad
- King Lear, W Shakespeare
- Nietzsche’s works
- How to be Sick, T. Bernhard
- The Sweet Spot, P. Bloom
- Thich Nhat Hanh’s works e.g. No mud, no lotus
- Reimagining Chronic Illness, Meghan O’Rourke
- The Obstacle is the Way, R. Holiday
- Perceptions in Pain, D. Padfield
- Books by H. Marsh (who is a neurosurgeon and writes from the view of a doctor, caregiver and patient)
- Anatomy of an Illness, N. Cousins
- A Still Life, J. George
- Fragile Lives, S. Westaby
- The Jataka Tales
- Acceptance, R. Frost
- and more
And finally some songs about pain:
- Pain, Three Days Grace
- Hospital Flowers, Owl City
- Flags, SYML
- Valley of Pain, B. Raitt
- Make It Go Away, S. Crow
- The Cure for Pain, J. Foreman
And songs to sooth the pain:
- Soul Smile, Yellow Days
- When We Were Very Young, Belle and Sebastian
- Hey Jude, The Beatles
- Simon and Garfunkel songs
- Move on up, C. Mayfield
- Float On, Modest Muse
- Hope, N. Bedingfield
More recommendations here.

Pain from a Buddhist’s Perspective
We should continue with pain from a Buddhist perspective. It opens a lot of questions.
We often think: ‘Pain and suffering come together’ or ‘suffering arises from pain’. When there is pain, suffering arises and to get rid of suffering (which is bad) we have to get rid of the pain. A Buddhist, however, wouldn’t agree to this conclusion.
The four noble truths lie in the heart of Buddhism:
- Dukkha, ‘life is suffering’
- the origins of dukkha, ‘suffering has a cause’
- freedom from dukkha ‘…an end/a cure’
- the path leading to its freedom. ‘The path to its end’
Where we may find suffering not only in physical or emotional pain, but also in joy since we know that everything is temporary.
Buddhists, in fact, differ between the suffering of suffering itself (e.g. from physical and emotional pain, a situation we find uncomfortable), of change (e.g. from joy as we know that it will be over at some point in the future, see also impermanence**) and of existence (as we never fully understand life in which suffering is inevitable).
Suffering should become optional, when we put our negative judgement towards pain aside. This is a very difficult task, speaking from my view as a chronic pain patient. My advice for chronic pain: Be curious (e.g. what exactly, what type, how big is it, how does it develop? etc) about the inner sensations instead of wanting them to go away. In the end, our mind and body are one, so let them work together. Isn’t it fascinating that we are more than our body and, hence, can REACT, ALTER our reactions? Our life shouldn’t evolve around pain. But often it does. It dominates the rhythm of the day. So why not transform it into something new? Ask yourself: How can I learn from this? What can I turn the pain into? Rather than: How can I get rid of it? (e.g. I am writing these poems, advice or my thoughts to connect with others, share my experiences, maybe help others; I use the pain to create something new and as my own therapeutic support… I am writing this fueled by my pain.) Also, I can explain it, I can come close to it and the pain is not something scary, I don’t need to be afraid of it. The pain does not control me.
My second advice is: Bring attention to your breath – a sensation beyond pain – you can focus on something else.
To get there, follow the Buddhist understanding of pain towards suffering. For mathematicians it basically can be defined as: Suffering = pain x resistance (may be easier to understand this way). Zero resistance means zero suffering (with resistance smaller one you can at least reduce the original amount of pain). But how can we reduce or let go of resistance?
Everything, and thus pain, is temporary since everything is evolving according to cause and condition in the interconnectedness of all beings (the temporary nature can be found in E. Dickinson’s poem mentioned above). Although, resistance makes our life much more difficult, sometimes it is even more difficult to let go of it. This is a human phenomenon. A good way to get rid of our everyday thinking, our static thinking, is to focus on our breath. Breathe out the resistance. We need to let go of the attachment to comfort where we want to get rid of everything that is ‘bad’ such as pain. Let go of your worries, your non-acceptance and the second arrow won’t hurt. (Have a look at Frost’s poem above for the importance of acceptance.)
Here is a sweet story or parable to understand what I am talking about: ‘The two Arrows’ or ‘The Second Arrow’. Every time discontent happens towards us, we are hit by two arrows and the second one is even more painful. Picture yourself walking in the forest.
In life, we can’t always control the first arrow. However, the second arrow is our reaction to the first. The second arrow is optional.
said the Buddha when he was asked: ‘If a person is struck by an arrow, is it painful? If the person is struck by a second arrow, is it even more painful?’ by one of his students. The first arrow is unavoidable, sudden and unexpected (physical pain, emotional pain, loss, grief…). To avoid the second one, we have to be (more) aware of the first one, accept it and take our chance to alter our reaction – it is in our hands. The second arrow hits us with a possibility of choice of reaction towards it. Be mindful and aware of this, at any time.
Moreover, as you will find out below, our sympathetic nervous system reacts towards pain and our reaction can amplify this process a lot, for example, our breathing influences our heart beat which again changes the perception of pain etc. Deep breathing and the focus on our breath can reduce our perception of pain. During deep breathing you have to your diagphragmatic muscles that naturally ‘massage’ your intestines.
To combat suffering, (breathing) meditation is an option. According to Buddha this is the noble eightfold path (right view: our actions have a consequence, right intention: love and compassion and good thoughts in the beginning of all, followed by right speech, right action, right livelihood through ethical work, along with right effort, and right mindfulness, to finally arrive at a state of right concentration: awareness***), practising mindfulness and awareness through good thoughts, words and actions; hence generating good karma and ‘better’ rebirth.
Practise deep breathing:
- Get comfortable, somewhere calm.
- Concentrate on your current breathing.
- Then start your deep breathing: Take a slow breath in through your nose and wait as long as it needs to fully fill your chest and abdomen. Then breathe out through your mouth, slowly and fully.
- Don’t focus on anything else than your breath.
- Repeat it as often as you like.
- Practise it daily. You can close your eyes, put your handy on your belly, this may simplify it.
Last, but not least, the idea of interconnectedness (as in Buddhism) always helps me during very painful phases. I know that I am not alone, but just one tiny knot in the vast net of all beings. Right now there are others that experience pain, too, and don’t know how to react; and there are others that experience a different form of suffering; and there are also beings that experience joy or beauty in this impermanent world. Pain grows into compassion and truly enlightens my body and mind in that particular moment. From a Buddhist view, pain develops (into) compassion for other sufferers and yourself (see also loving kindness compassion and meditation).
Often in our Western mindset we want to see the whole picture, the whole stair. But we should be grateful to be on one step and concentrate on this step only. This needs a lot of trust. Trust in yourself, your environment, the whole net. The acceptance for the moment only changes your whole understanding. You will find another dimension inside yourself, a dimension of deep consciousness. The second arrow is the uncertainty of all possible effects of the first arrow. We might worry about the pain itself or its consequences for us or the environment, our loved ones. Let go of it. Only then pain can teach us and make us wiser.
This post will evolve about pain, specifically the ‘medicine’ behind pain. You can skip this part, below there are some fancy recommendations.


Definition of Pain
Pain is defined as ‘an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage’ according to the IASP **** and a ‘personal experience that is influenced to varying degrees by biological, psychological and social factors.’ according to the European Pain Federation.
These definitions already show that pain is something complex, influenced by psychological, emotional and biological components. Pain is subjective and may be described as an invisible illness/symptom itself and/or consequence from another condition. In fact, the question ‘Symptom or disease?’ may be a major question in its classification as often it is a result of another underlying illness, but can dominate the patient’s life and can become an own identity.
Pain, especially chronic pain, can decrease the patient’s quality of life and may affect general functioning.
The word ‘pain’ derives from Latin ‘poena’, meaning ‘penalty’ or ‘punishment’, and similar meanings in other languages.
Biology
Let’s start with its biological component. Pain is an important part of the ‘fight or flight’ response and has helped animals and humans from the earliest beginnings. Pain protects and warns us. It helps to prevent (further) damage. Unfortunately, sometimes pain loses its actual task and pain signals are transmitted without actual or potential damage.
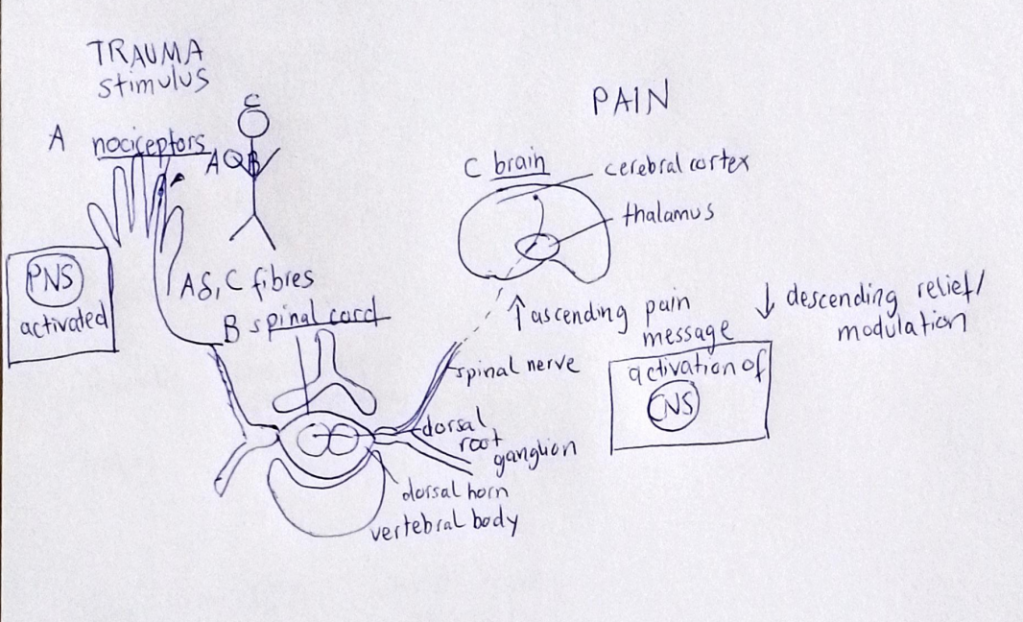
Pain does not equal nociception (there is pain from nociception, but also without*****). In the former case, physiologically, pain is caused when nociceptors (nerve endings) come in contact with stimuli that are noxious i.e. that are strong enough to cause damage to the body. From these special receptors in the peripheral nervous system (PNS) the signal is then processed and decoded in the central nervous system (CNS).
They can be categorised according to its nature into:
- thermal (due to heat or cold),
- mechanical (e.g. due to an acute injury, often affected by movement and/or position),
- chemical (e.g. inflammations changing pH)
or by location:
- skin = superficial,
- muscles/bones/tendons/ligaments… = deep somatic,
- organs =visceral
or by nerve conduction speed/diameter of the two major fibres that conduct pain:
- A delta (myelinated [= with a layer of insulation] afferents with medium diameter [2 to 5 micrometre] that mediate acute/immediate, well-localised, sharp pain) also named as group III afferents and
- C (unmyelinated [= no further layer] afferent thinner fibres that mediate slow/delayed, poorly-localised, dull/aching pain) also known as group IV
where afferent means carrying information toward the centre of the body. The former has a bigger diameter and faster conduction velocity compared to the second one. Thus, the fibres of fast pain.
These signals are not attached to any judgement nor emotion or feeling and it is not pain. It only means that it is strong enough to jump the synaptic gaps in the nerves to the spinal cord and then to the brain which receives the message. Afterwards, the brain decodes or rather decides along with other factors whether there is pain. This is the subjectiveness that is part of our pain perception. Pain does not always equal 1-1 its damage.
For example, when there is repeated nociception (as in some chronic illness conditions), the patient ‘gets used to it’ and even weaker messages are able to jump the gap. This is a major issue in chronic pain patients that needs to be tackled through different methods mentioned below. Here we see that pain is not only related to sensory neurons, but our subjective experience.
Aside from the nociceptive mechanism (damage of tissue), there is also
- neuropathic (from nerve damage),
- nociplastic (central sensitisation; pain not related to its actual damage, often widespread, more intense than expected) and
- somatoform (no physical cause can be found) pain
that can all show alone or combined in patients. It is very important to understand which form of pain is the (main) acting one since they are treated differently (e.g. for the last two forms patients won’t benefit from an increase of pain drugs).
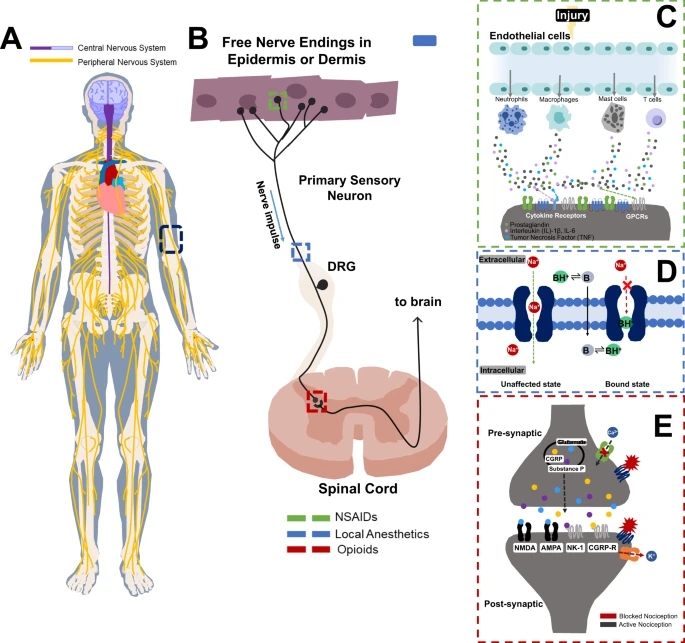
Injury in the PNS, from the nerve endings the nerve impulse is sent to the spinal cord and then to the brain (CNS). Here you can also see the function of NSAIDs, local anaestehtics and opioids. For example, opioids suppress the pain signals in the central and peripheral terminals.
source: Brigham, N.C., Ji, RR. & Becker, M.L. Degradable polymeric vehicles for postoperative pain management. Nat Commun 12, 1367 (2021). https://doi.org/10.1038/s41467-021-21438-3
Lastly, one can also categorise according to the pathways of the pain:
- Primary sensory neurons (in the PNS, signals are conducted from the periphery to the dorsal root of the spinal cord),
- Secondary sensory neurons (in the spinal cord or brainstem, signals are conveyed to the thalamus) and
- Tertiary sensory neurons (in the thalamus, signals are transmitted to the somatosensory areas of the cerebral cortex).
Hence, there are three ‘layers’, the periphery, the spinal cord and the brain with the thalamus, to recall.
In the neuroscience of pain, neurotransmitters (= messenger) also play an important role. When the brain has received a signal it can react by sending a signal back. It can release natural painkillers (known as endorphins), increase the immune response or send other neurotransmitters that alter the pain. Again, there are a lot of unanswered questions regarding this topic, but it is assumed that we all have different types of neurotransmitters leading to different sensitivities to pain (basically due to our genes). Glycine (probably the simplest amino acid), for example, is an inhibitory (= inhibits signals) neurotransmitter of the CNS that can potentiate the action of glutamate at N-methyl-D-aspartate (NMDA) receptors. NMDA receptors are normally regulated by its agonist glutamate, probably the most popular neurotransmitter for pain modulation (especially for acute pain), and are found in various locations as transmitter and modulator of pain in inflammations and tissue injury. Serotonin (5HT) is important in chronic pain, many medications treat (especially somatic) pain disorders with selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) as well as a communicator between the brain and the gut (prokinetics such as Resolor are based on this). Others are substance P (can modulate the transmission of pain information from the periphery to the CNS), histamine 1 (in visceral and somatic pain important), vanilloid type 1 ‘TRPV1’ ( colorectal mechanosensation and pain from inflammation) and opioid receptors (in myenteric plexus, including visceral nociception), voltage gated channels (stimulated by tissue damage; for example, potassium channels, which when blocked can reduce hypersensitivity in the periphery) and more.
Different Types and Assessment of Pain
For its treatment, it is not only important to understand the mechanism behind, but also the perception of the patient. Pain always involves a physical and psychological component that both need to be dealt with.
In practice, acute and chronic pain is defined from its duration. The former resolves quickly (definitions differ from 30 days up to 6 months) and is caused by sudden injury, surgery etc, the latter is persistent (i.e. longer than 6 months) and usually has a gradual start from an illness or simply continues. Here, I want to focus on chronic pain which is much more difficult to treat. It is not always easy to distinguish between both e.g. whether the patient has a ‘chronic pain flare up’ or an acute condition.
The classification of pain can also be according to
- the region of the body involved (e.g. abdomen),
- the system whose dysfunction may be causing the pain (e.g. gastrointestinal),
- duration and/or pattern (e.g. chronic with exacerbation periods),
- intensity and
- its cause (e.g. Crohn’s inflammations).
The underlying illnesses of chronic pain patients vary across countries and specific subgroups (e.g. older vs younger adults), but spinal pain (particularly, low back pain), headaches, osteo/arthritis, cancer and post-surgical pain are the most common. Fibromyalgia (widespread pain) and neuropathic pain conditions have grown in the past years. There might be more due to unrecorded numbers, but about 20% in the EU have moderate to severe chronic pain.
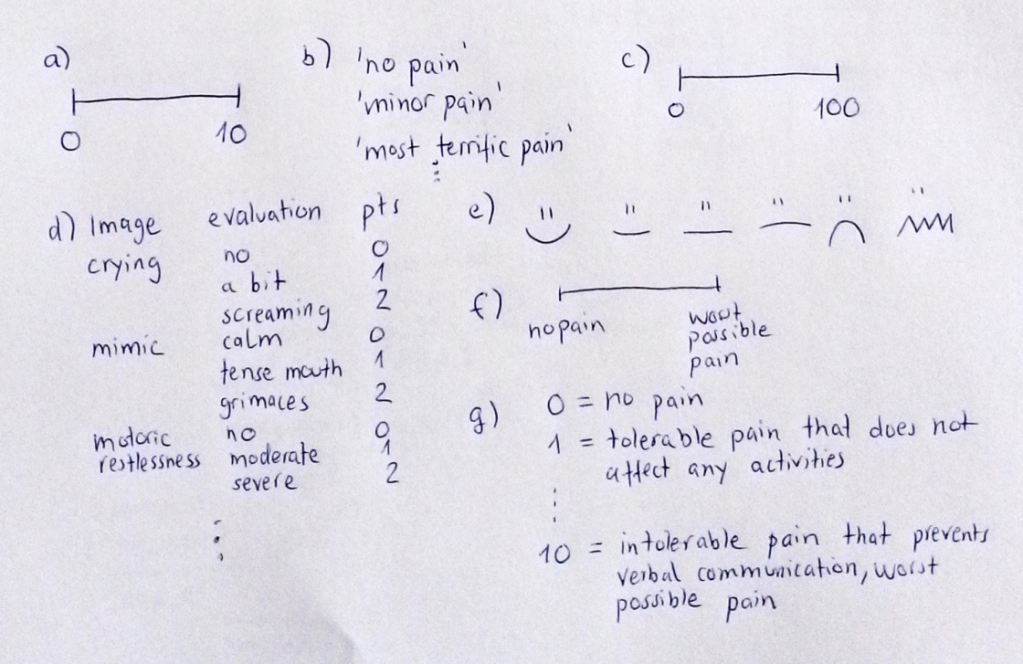
Everybody who has been a patient due to illness knows that the doctors ask about its intensity (e.g. 1 to 10), its quality (burning, shock-like etc) and its evolution (getting worse, at night worse etc). Along with other tests results and diagnostics this is very important to find the cause and/or a possible treatment option. Therefore, the classification of pain has been a major topic in pain research, and so has its assessment.
Doctors use a broad range: verbal rating scales (VRSs), numerical rating scales (NRSs) and visual analogue scales (VASs).
Your pain cannot be felt by others nor can it be objectively measured, both qualitatively and quantitatively. Thus, we are dependent on an indirect way through self report and/or physiological and behavioural observation strategies. Obviously, in some patients such as babies or patients with severe dementia, a proper self-report is very difficult. Hence, doctors and nurses analyse their breathing, mimic, body language etc.
Whether you participate in a chronic pain patient programme or get admitted at an outpatient pain clinic, during the admission process you will need to fill out a pain questionnaire that deals with all kinds of questions regarding the above mentioned categories as well as the therapies that have been tried so far and whether they have improved your pain. This includes multiple choice, drawing locations, answering questions about the pain itself, but also its effect on your quality of life quality, work, social life etc. See, for example, the McGill Pain Questionnaire. Here is a typical German Schmerzfragebogen. During clinic inpatient stays patients are usually asked about their pain level (0 to 10) twice a day (morning and evening round) along with vital levels and co such that the doctors can analyse the patient’s pain evolution and the nurses can ring the doctors when the pain level is too high.
Consistent assessing and documenting is key, pain treatment should adapt according to it. Re-assessment after every intervention might be useful in documenting progress and adapting treatment again. For example, if the patient talks about ‘electric, shock-like’ or ‘burning’ pain, he likely suffers from some kind of neuropathic pain e.g. neuralgia; ‘dull’ and ‘during moving’ often suggests myofascial involvement; ‘throbbing’ often goes along with migraine and an obstruction is typical visceral pain.
Visceral pain is caused by ‘nociception of the organs’ (thorax, abdomen and pelvis) due to their damage, inflammation or injury e.g. pain from an ileus or gallbladder stones/colics. Often patients describe it as dull or achy, deep and diffuse pain, in most cases patients find it more uncomfortable as pain arising from other causes such as myofascial pain. Functional GI disorders or dysmotility conditions come along with chronic visceral pain. The brain-gut axis communication and, thus, the exact mechanism of visceral pain is not completely understood. When the underlying problem, the lack of motility, cannot be improved, pain management is very difficult to handle. The intestines themselves don’t have any specific pain receptors, but certain threshold systems. For example, lack of motility leads to stagnation of fluids and air which lead to dilatations of the intestines. Above a certain limit of stretching, the patient perceives abdominal pain. Abnormal contractions (as in obstructions due to a mechanical issue and in pseudo-obstructions due to enteric neuropathy), ischemia (= lack of blood flow to the intestines)and mucosal irritations all lead to qualities above their threshold. Visceral pain is influenced by many other factors like hormones, organ functions, general pain perception etc.
Further important terms to mention, are
- Allodynia: pain due to a stimulus that normally shouldn’t provoke pain,
- Hyperalgesia: higher sensitivity to pain stimulus,
- Hypersensitivity: increased response to a stimulus
GI disorders like dysmotility often come along with visceral hypersensitivity, patients suffer from chronic abdominal pain that often is very difficult to manage.
Pain truly is a fascinating topic. There are pain conditions that include the whole range of possibilities, from the impossibility of feeling pain to severe pain conditions due to allodynia or similar including congenital insensitivity to pain (CIP), hereditary sensory neuropathies and hereditary sensory and autonomic neuropathy (HSAN) (when autonomic nerves are involved, too) as well as acquired ones such as fibromyalgia. The SCN gene mutations play a key role in the sensitivity of pain. Those genes are important in the channel build up for the transport of sodium ions which can alter the signals of pain mentioned above. This family of genes should be analysed when patients experience such conditions. Visceral hypersensitivity is a major problem in GI disorders. The constant stimuli (e.g. dilatation of the intestines from the lack of proper motility or repetitive ileus states) lead to an increased response such that the patients suffer from intense chronic pain (that does not always correlate to the actual amount of physical problems in that phase). Often patients find themselves in vicious cycles of unrelieved pain or pain improvement through medication that increase the underlying problem (see below, opioid treatment). Hopefully, there will be more research on the cellular level and exact mechanisms such that therapy options including more efficient drugs can be developed. I will give some further insight in visceral hypersensitivity and its management in a future post (since I am a sufferer from it myself).
Have you understood everything?
- Does pain equal nociception?
- Sort the illnesses to their classifications of pain and find some words for its typical character: Arthritis, nerve damage, depression, acute ileus, SCN9A mutation, CRPS
- What three important locations do the different pathways of pain include?
- What kind of nociceptive stimulus is this: Acid over your hands, burning in hands and feet in Diabetes patients, chilblains, when you fall down the stairs and break your leg, when you twist your ankle, a burn, a car accident
- What was the original function of pain?
- A patient with severe dementia groans loudly and hyperventilates, he is very tense. How strong is the pain?
- Which fibre transports easy-localisable, fast pain?
- What kind of rating scale are these?
Further information can be found here:
- IASP Merskey H, Bogduk N (1994). Classification of Chronic Pain (2 nd ed.). Seattle: International Association for the Study of Pain. pp. 3 & 4
- Rosenow JM, Henderson JM. Anatomy and physiology of chronic pain. Neurosurg Clin N Am. 2003 Jul;14(3):445-62, vii. doi: 10.1016/s1042-3680(03)00009-3. PMID: 14567145
- Institute of Medicine (US) Committee on Pain, Disability, and Chronic Illness Behavior; Osterweis M, Kleinman A, Mechanic D, editors. Pain and Disability: Clinical, Behavioral, and Public Policy Perspectives. Washington (DC): National Academies Press (US); 1987. 7, The Anatomy and Physiology of Pain
Treatment
For acute pain issues that don’t need intervention or milder chronic conditions, many people can self-manage the pain via rest or exercising, lifestyle adaptations, natural remedies etc. At some point, however, everyone needs professional support. More than 50% of A&E cases are due to pain, many of them again due to an already known condition.
In order to treat (chronic) pain, all factors have to be dealt with. The ‘biopsychosocial approach’ tries to include the complex interactions of biological (genetic, biochemical etc.), psychological (mood, thoughts, prejudices, etc.) and social (cultural, familial, socioeconomic, etc.) factors which again are different in every patient.
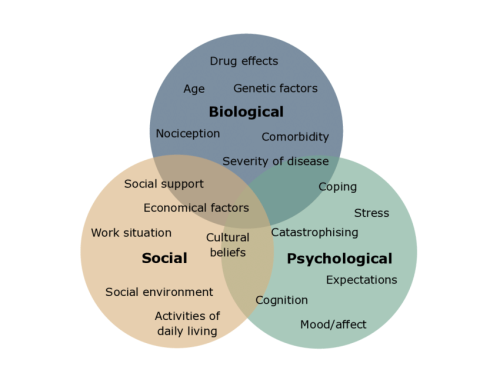
Biopsychological approach model and examples for the three main factors, for example, age and genetics as biological factors. Treatment should include all factors including their interactions i.e. the wole diagram whereas often treatment consits of the biological circle only (without the factors’ interactions).
source: https://europeanpainfederation.eu/what-is-the-bio-psycho-social-model-of-pain/
Pharmacological approaches are based on medicines or medical therapies (drug schemes, TENS, opioid treatment, nerve blocks, pain pumps, surgery…*******), non-pharmacological approaches deal with altering the perception of pain through exercise, physio-, osteopathy, meditation, Yoga, cognitive behavioural therapy, psychotherapies and more.
Patient education is important in all pain conditions.
For people with long-term pain conditions it is vital that they have access to an outpatient pain clinic, pain programmes, inpatient care or an admission to a pain rehab centre or inpatient pain management when necessary and a range of pharmacological and nonpharmacological approaches adapted to the individual patient. However, this is not often the case. Most of the time, doctors follow the biomedical approach only, the primary care (and A&E) are the only supporting ‘specialities’.
Alternative medicine such as TCM (Chinese medicine), acupuncture, certain massage techniques and more can be good (additional) support since often they are less invasive (thus, less risks that might amplify the pain or cause further [pain] problems) than our Western approaches. From my own experience, I can recommend TRE (‘Tension and Trauma Releasing Exercises’) which is an accumulation of exercises that can potentiate ‘shivering’, hence, also the name ‘neurogenic shivering’, which brings our body and mind back to a balanced state. It is believed that tension (through physical, but also emotional pain or stress) and trauma (all kind of trauma, including accidents, injuries, violence etc). More information, including the exercise can be found here (German), (English), directly to the exercises. Animals and humans react towards trauma with rigidity, followed by shivering/shaking to release the shock. The TRE developer interprets this shaking as a healing process. The exercises include various muscle regions, for example, the psoriasis muscles, that contract themselves when we experience a traumatic event in order to protect our vital organs. Many of us, with or without chronic pain have tense muscle there (i.e. I can recommend those exercises to everyone – everyone carries some kind of trauma in his/her body and mind).
Complementary medicine also provides a range of support through natural remedies, herbs or dietary supplements e.g. prebiotics or probiotics. Yoga, Tai Chi, Qi Gong and co help actively to combine body and mind where breathing becomes key (see also above, in Buddhism). And even, when those alternative options don’t reduce the pain itself, it helps with the anxiety and other negative feelings that come along with it.
When the pain is related to an underlying condition, it needs to be treated (when possible) – also with the aim of reducing the pain. For example, pain from inflammations in IBDs may be improved by immunosuppressive therapy or surgical interventions; pain from dysmotility such as STC may be treated by increasing motility and surgical intervention should be weighted against conservative therapies.
Depending on these underlying factors a multidisciplinary approach must be found. This includes doctors from different expertises (specialists for the underlying condition, pain management, anesthesiologists, physio, psychologists etc). Communication between patient and doctors as well as between specialties is essential. In a pain rehab clinic, for example, patients participate in single and/or group talk therapy sessions, physio, education sessions about the mechanisms and coping strategies of pain and individual biomedical approaches. Various treatment options are probed, body awareness exercises are taught, the doses of meds are (slowly) altered and patients learn how they can manage the pain at home, at work and other tips and tricks. ‘Small’ helpers according to the underlying pain condition are introduced that can be continued after the clinic and alternative options are tried out e.g. TENS, heat/cold therapy etc. Even when you have lived many years with pain and have developed your own coping techniques, I would recommend participation in such a programme when you feel stuck with your pain. Many times, this is the only way that the patient can be treated as an individual and a variety of possible treatment options can be tried out and adapted. When possible, look for a centre that also includes some expertise in your illness. Unfortunately, not many clinics offer interdisciplinary pain management.
My second recommendation is biofeedback which is a non-invasive method to show the patient his/her body’s processes. Via electrical signals (EMG or EEG) the patient’s heart beat, muscle tension, temperature, etc (all indicate some level of stress) or brain activity or other are measured and shown to the patient such that he/she can follow how signals change according to factors like breathing. In certain dysmotility disorders it might be useful to show sphincter muscle tone or other related tones that can present GI motility, in pelvic dysfunction or urinary incontinence or neurogenic bladder dysfunction the pelvic floor tension can be shown. After a few sessions the patient becomes more aware of his/her body function and can then reduce the pain related to it or even improve its function (which also improves pain usually). It can also be combined with other techniques of relaxation such as deep breathing, meditation or progressive muscle relaxation (muscle groups are tensed and relaxed in a specific order, the patient becomes more aware of the tension in his/her body and becomes overall more relaxed afterwards).
Psychological help can be given through meditation, body awareness, exercises, cognitive therapy or talk therapy, alone and in groups. Many patients benefit from distraction, whether it is through focusing on a (new) hobby, a special therapy (e.g. art or music therapy) or by certain strategies (e.g. muscle relaxation). Some patients also recommend hypnosis as a tool, especially, when the pain has an emotional part or when the pain is related to some kind of trauma.
The WHO has a step-like medication scheme where the recommended medication for pain management ist given.
- Level 1: non-opioids, including other drugs like non-steroidal anti-inflammatory drugs (NSAIDs) e.g. Ibuprofen, ASS or COX inhibitors, if the pain persists:
- Level 2: weak opioids (plus co-analgesics) e.g. tramadol, if the pain persists:
- Level 3: strong opioids (plus co-analgesics) e.g. fentanyl, if the pain persists:
- (level 4: further interventions such as nerve blocks, pain pumps etc)
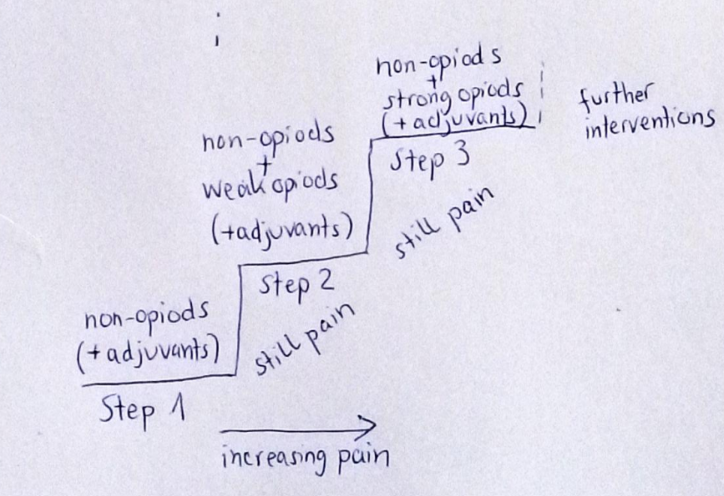
Co-medication is used as additional support and should decrease side effects of opioids (mainly antiemetics for nausea and laxatives for constipation where the patient gets used to the former). For example, low doses of antidepressants can help with (physical) pain procession, anticonvulsants help in neuropathic pain, muscle relaxants reduce spastics, dexamethason inhibits swelling etc. Often, in chronic pain management one uses a trinity of opioids, some kind of level 1 drugs and co-analgesics such as antidepressants.
Opioid treatment in severe pain cases has been a major issue in the past decades (in the US also known as opioid crisis). There are many conditions that are treated with long-term opioids, although there are contraindications or they are inefficient (there are no proven facts that opioids help long-term in non-cancer pain) or not needed. Compared to other drugs, opioids are often the best in reducing pain and also don’t have any long-term effects on our organs. Nonetheless, opioids have severe risks, short-term such as constipation, slow breathing (that can lead to hypoxia) and long-term risks, especially dependence (which is different from addiction). There is a huge difference in the intake of opioids due to severe pain or due to abuse/getting high, but the final problem is the same: getting off the opioids is a difficult problem and medical assistance is needed. There are specific guidelines to prevent such problems, but often doctors (especially when patients are only treated by their primary doctor) don’t necessarily follow them.
Unrelieved pain causes a biological stress response including an increase in metabolism and a decrease in cellular immune response. The endocrine system reacts to unrelieved pain with an increase in hormones and catabolism. Along with the underlying illnesses it accelerates weight loss, can cause or increase tachycardia, breathing problems due to an increased respiratory rate, fever and ultimately can indeed lead to shock and death. Further, it activates the sympathetic nervous system (hence decreases all parasympathetic functions such as digestion) and suppresses immune function which again accelerates more problems. Hence, aside from the misery of unrelieved pain for the patient and his/her quality of life, there are true harmful physiological effects that shouldn’t be ignored. (Plus it is a major effort and high costs in health care.)
Psychology of Pain
Pain perception depends on many factors, nociception (or other physiological mechanisms) is only the ‘start’. We can alter our perception with our emotions, level of stress and behaviour that are dependent on our previous experiences and our belief or anticipation of potential consequences. Along with our sensory input, nociception becomes pain, a fully subjective experience.
The more you try to avoid it, the bigger suffering is. Hence, acceptance is a major step in successful pain management. Negative states of mind such as sadness, hopelessness, grief or anger usually increase pain perception.
Always recall: It is not your fault and you are not your pain. Yes, pain can change you. It interferes with daily life, career perspectives, relationships etc. But don’t let it dominate your life or you. You are still the maker of your life, so don’t stay inactive or get stressed out from it, don’t lose hope.
Whatever can improve your state of mind (distraction, focus on your hobbies or focus on breathing exercises etc), do it in order to improve pain perception, too.
Pain is not measurable or detectable in tests. It is inside you, sometimes invisible. Therefore, it is your task to open up about it (as much as you want to) to your doctors, but also your family, friends and loved ones. Don’t isolate yourself with the only burden you have.
Alter your reaction towards pain, because you have the possibility to do so. You might be unable to change the illness that causes nociception, but you can change the perception.
Often, patients undergo endless testings and doctor visits until they are diagnosed with a (physiological) illness. Throughout these years of uncertainty and inexplicable pain, doctors might suggest that the pain does not exist, that psychological help is needed. It is true that in some cases no organic issue can be found, but, nonetheless, the patient does experience pain and this needs treatment according to it. Physiological illness and the burden it brings (not only pain) can also introduce ADDITIONAL psychological burden and perhaps illnesses such as depression which then also needs suitable treatment. In my opinion, every patient can benefit from psychological support. We have to carry so much with us, pain, other symptoms, the effects they have, uncertainty, unpredictability, … for many of us, the illnesses have turned our life upside down and we have to adapt to new conditions. We have to let go of our older self, ambitions, friends, sports and so much more. It can help a lot to talk about all that with a professional counsellor.
An efficient method to shift the focus away from pain is cognitive behaviour therapy which is a type of talk therapy during which the patient becomes more aware of his/her negative thinking. Often we have already gotten used to certain static ways of thinking (which leads to certain ways of actions) that we aren’t aware of anymore. For example, when someone has experienced bad pain flare ups during the night, he/she is likely to think that it will happen again during the next night and simply the expectation of it can lead to the inability to fall asleep or urges the intake of pain medication before any pain is actually happening. You can talk about your feelings and thoughts to an experienced therapist who will help you to deal with them in a better way: Identification of the problem, acceptance, awareness of your thoughts and beliefs and their relations to the problem, identification of negative thinking, and finally reshaping of those thoughts. CBT can also help with other problems that affect daily life negatively due to the development of certain destructive thinking e.g. in obsessive compulsive disorders.
What makes pain worse?
- Attention (focus on pain)
- Anxiety
- Stress
- Anger
- Bad previous experience (which you let dominate your anticipations)
- Catastrophising
- Lack of mobilisation or activity
- Complete isolation
All scientifically proven!
Recommended book: Linji’s Achtsamkeitslehre (German) where the privilege of a rational thinker and mindful observer, both united, is depicted. Together pain can be managed by keeping distance to see clearly.

What Pain can Teach us
Apart from the fact that pain is essential for survival, prevents (further) damage etc as explained above, pain is vital for life and the understanding of its beauty as well.
You can use your pain to create something new or as creative inspiration e.g. for poetry, art or music. Pain helps you to grow. It helps in the development of your character. As a major challenge, pain forces you to rethink your style of life, adapt your aims and strategies of problem solving.
Pain teaches you to be more mindful about the body and life in general. It helps you, or demands you to listen to your body. During this process you will find gratitude. You cherish little things, small moments, the good times, better times…and also the ‘bad’ times during which you receive support from the medical system, your loved ones and strangers.
Pain is a reminder about our fragility and what truly is important to us. There are priorities to choose, because pain takes up a lot of energy.
Chronic pain has taught me how to adapt and how to appreciate. I know what helps me and I also know who is good. No matter how cruel this sounds, I know what or whom I have to get rid of.
Animals feel pain. Bo always knows how I am feeling. Pets are good companions, in good and bad times. Focusing on them is a great distraction and having a responsibility doesn’t allow you to let go of life. There are interesting studies that prove that pets sense physical and emotional pain. They seek physical contact which in turn improves our state of mind. They stay with us throughout the most misery flare ups and everyone is grateful for a companion in these times. They see our faces, our body language and our smells (probably the best pain assessment in the world). For example, they can evaluate the smells of elevated cortisol levels (= increased stress level) and/or low serotonin levels (= good mood) in contrast to our everyday levels. Thus, they especially feel pain in their owners.
You also become good at describing your pain and hence emotions in general. Your communication improves. You become better in analysing your own emotions, better in self-compassion, and also in compassion and empathy for others. Pain makes us realise that we are not ‘immune’ to nature and that we can only support each other. Pain reminds us of our human nature and our humanity.
Pain definitely is a better teacher than happiness. In Nietzsche’s words ‘pain makes us stronger’. You have to listen to your pain and it will give you a lot of answers and advice. But you don’t have to follow them. Pain can push us beyond limits we didn’t know existed. Be careful and pay attention. Pain is a teacher as it contains major information.
Finding a purpose in pain not only improves pain perception, but gives your life (more) sense again. Whether it is the inspiration from pain, your religion, supporting others or your development from it, it helps your healing process tremendously. In fact, pain may awaken that very purpose. The moment you find its purpose there is no more suffering.
If pain wasn’t such an *** it would be the most beautiful on Earth.
What’s the Point?
It would be efficient for everyone, the patients, their loved ones, carers, doctors, …health care (pain management is very costly – a good amount of hospital admissions is due to insufficient pain management, some say more than half of the emergency visits) if the usual pain management strategies would change to a broader, multidisciplinary approach.
There needs to be more awareness and education, especially through increased communication between patients, carers, doctors, across levels…
More resources can be found here:
- European Pain Federation: ‘The overall vision will be to optimise understanding and management of pain through promoting high-quality, collaborative basic science, translational, and clinical research.’
- Pain connection, The Mighty to find support
- American pain societies: US Pain Foundation, Chronic Pain Association
- The Journal of Pain Research (official journal of the American Society of Pain & Neuroscience)
- Schmerzliga, deutsche Schmerzgesellschaft, UVSD in Germany
Research in pain physiology and management is vital to answer questions like: How does our past experience shape our current pain perception? Why are there different levels of pain perception and sensitivity? How can we combat chronic pain more efficiently or how can we prevent chronic pain at all? Experimental pain research, biology, medicine, psychology have to look into specific pain mechanisms, new drug schemes beyond opioids, improve the understanding of individual pain perception and central sensitisation etc.
Pain is multifactorial and multidimensional and it needs to be dealt with accordingly.
Moreover, we need individual treatment plans as pain is subjective. There is not only a medical/scientific part, but an emotional one as well. Psychological support is essential.
The access to individual pain treatment is equally important meaning we need pain rehab centres, chronic pain clinics, outpatient doctors etc throughout the countries. When patients have to live many years with the same pain due to long waiting times or lack of resources, the pain can manifest itself and turn into chronic pain which cannot be eradicated anymore.
We need an increase in pain research, education and awareness!
And us patients have to be viewed, evaluated and treated as a whole. Pain is a dynamic process with many factors, complex interactions, that cannot be found in books. Doctors have to listen and talk to us patients very patiently.
And so do we. We have to accept our conditions and live with the pain.
My top tips for chronic pain, be aware that:
- Suffering and pain are distinct*****. And nociception and pain are distinct.
- Distraction can help you through the most painful flare ups. Use either problem focusing (as there is something you can change), a hobby (reading, writing…) and/or breathing (meditation).
- Pain isn’t a threat nor do you need to be afraid of it. Come close to it. Listen to it. Don’t be afraid.
- You know your body best. (Is it another major flare up or an acute emergency that needs treatment? Should you rest now?)
- We should meet pain as a community, despite its individuality, you are not alone! You can ask for help and you can support others. You may join a support group.
- Observation without judgement is key. Let go of all negative emotions towards pain.
- You may develop your own coping mechanisms according to your feelings and needs. Evaluate your pain and your reaction towards it. Analyse all its details. Adapt. Change your reactions as your pain develops.
- Isolation won’t make it better. Sometimes it feels as if everyone around you gets used to the pain except you, sometimes it is the other way around. Try to talk to your loved ones, family and friends about your feelings. And if you want to be alone, don’t feel bad about it. A professional therapist might be useful.
- Negative thoughts lead to negative actions and make your pain definitely worse. Optimistic thoughts might turn into disappointment or unrealistic expectations you(r body) cannot fulfil. Keep a realistic mindset.
- Boost your endorphins, natural pain killer, by exercising or at least mobilising.
The Perception of Pain
As already explained, pain arises from two neural paths: The signal that comes from somewhere in the body and activates the cortex of the brain (the anterior cingulate cortex), followed by the perception of pain. The second path is given by the addition of our feelings, emotions, anticipations (probably involvement of the medial prefrontal cortex and the n. accumbes) which results in completely different reactions and sensitivities to pain. Also, further factors such as social, cultural ones, the environment and its situation, the patient’s personality as well as the understanding of pain/the underlying condition etc play an important role. Exploring the exact mechanisms and factors of pain perception is very important in the build up of new pain management strategies and drugs.
When pain has lost its function as an alarm or no organic cause can be found, one should look further into those other factors that may amplify the pain.
Nociception can occur without the awareness of pain (e.g. when under severe shock in accidents) and pain can occur without any nociception (e.g. phantom pain where the limb is gone and cannot hurt anymore).
When there are so many factors modulating pain, then we should find equally many alternative ways to deal with pain.

My own Experience With Chronic Pain
My own experience with pain is written down in the poem in the beginning of this post.
As if there is only pain on each step, behind and infront of me and in the moment. Only pain. But I have to climb it, it is the only way. As I am writing ‘You don’t have to fight against it, but you have to find a way to live with the pain’, I haven’t stopped fighting.
There are times where I beg and I just cannot ‘go on’. Where the pain is too severe. ‘You are so strong.’
And if I then hear this phrase it is as if I need to come up against some expectation I simply cannot. Sometimes we cannot be strong, sometimes we are weak. And that’s ok. Pain is a part of my life. Acceptation has been the best I could have done.
So that’s my first recommendation: Accept your situation.
In the past years I have lived with all kinds of pain: acute after major abdominal surgeries, mechanical ileus and gallstone colics; chronic due to vascular compression, CIPO and adhesions. I have had acute pain teams supporting me, I have an outpatient chronic pain doctor, I participated in various pain programmes and I have collected my own coping strategies including exercises, abdominal massage, meditation, focus, distraction and much more.
Everybody is different. Hence, it doesn’t make any sense to describe in detail what measurements have helped, but I hope that I have given you a broad overview about all the options in this post. Moreover, pain is dynamic. A drug that once worked for you may not work a year after.
Obviously, for diagnostics and treatment some kind of guidelines are necessary and I definitely recommend following them with your doctors. But pain management has to be individually adapted to the patient. Thus, I cannot emphasise enough to look for specialists that treat you as a whole.
It is the body AND the patient (without the illness) AND the illness along with many other factors interacting with each other that needs treatment. One measurement may work on me, but has no effect on you, although we may both have CIPO.
Pain management is even more difficult when the patient has a rare underlying condition or a still unknown illness.
Take me as an example, I have a rare underlying condition (dysmotility due to enteric nervous system damages), I have both enteric and autonomic neuropathy, I underwent a very invasive and exotic surgery in 11/2017 which has caused a lot of other complex interventions – both of which are very difficult to understand. Is the pain coming from nerve damages? Is it the adhesions? Is it the ANS?… I am very grateful that there are pain specialists that want to help me – give the list of diagnoses and past interventions. However, I haven’t found a doctor that completely understands my conditions and knows how to treat the pain in THIS setting.
Ideally, a multidisciplinary team should treat any complex cases. Doctors from expertises should communicate (for example, non-opioid treatment in dysmotility issues; radiology and gastroenterology can give feedback to the pain specialist about the dilatation of the intestines causing visceral pain i.e. neuropathic pain relief isn’t the first option etc). It simplifies the life of the patient a lot. However, I am very well aware that often this isn’t the case due to the lack of resources. As a patient we have to get active and ‘force’ our doctors to communicate or function as communicators. Thus, try to learn and understand as much as you can about your condition. In smaller clinics the expertise isn’t always that broad and deep, but the personal connection to the team might be closer. During the stays in the university clinics pain management after surgery was usually well planned. Someone was on hold 24/7 (pain catheter, spikes etc). But for chronic pain patients a more intense treatment is needed, ideally near home. Thus, it was a very good decision to start an independent outpatient treatment with a pain doctor who supervises the development over time.
Along with the previous factors I am also a person who has undergone major traumatic events in the past years (from horror hospital stays, to being at the edge of death, very discomforting interventions, the constant decline…) and I am Evita who was an active runner and strong-willed theoretical physics student, a curious scientist, part-time philosopher, crazy adventurer and explorer, someone for whom ‘nothing is impossible’ was the motto of life. This ALL accounts for chronic pain perception and possible treatment options. Don’t lose yourself in pain or its treatment. You are not your pain.
Once I had a good conversation with an anaesthetist, he correctly emphasised that doctors most often treat the bodies of their patients. However, in those bodies there is a mind/psyche/(whatever you may call it) living which we don’t understand. The flow between this ? and the body has a major effect on treatment options and outcomes. The same pain is felt differently, both in quality and intensity, even though it may be the same on a physical level. In fact, it may be the same input, the same stimulus, the same necessary impulse, the same amplitude of evoked potential, the same speed and paths to the spinal cord/brain stem and all other factors mentioned above may be the same, but, nonetheless, the pain felt won’t ever be the same. We have all different experiences and backgrounds. We have different life perceptions, anticipations, views and coping mechanisms. And exactly this phenomenon should be used to live with the pain.
In the treatment part I have listed a lot of possible measurements. Nature has been one of the best remedies for me. The tranquillity and calmness, the fresh air that literally invites me to practise meditation and awareness, past memories of my runs through the woods and the simple connection, the earthy ground(edness) all combine to create a wonderful, warm and safe feeling.
Trust in my body, trust in my mum, my doctors, treatment plans and trust in possible recovery has taken a lot of stress and fear that come along with chronic pain.
The unpredictability and uncertainty of pain have been huge obstacles for me as I love to plan and follow my plans (there are times I love surprises and adventures, but not necessarily the ones we had in the past years), I love to calculate and follow certain steps until I have a distinct solution, I prefer ratio over emotions and I want to keep control over my life… I still haven’t achieved the acceptance of pain’s unpredictability. I want to keep control over things even when I am in a very bad shape. I still have a lot to learn. Relaxation techniques as mentioned above have made this battle and frustration inside me a bit easier.
Pain has taught me a lot. Without the pain I wouldn’t have grown such a deep bond with my mum. I wouldn’t have started writing this blog. I wouldn’t have started meditation or practised mindfulness in the way I do it today. I wouldn’t have looked into body awareness. I could list many more positive effects that have their roots in my pain.
I am much more grateful than before pain was part of my life. For the life I had before and the life I have now, the support and love I receive and the options life still offers. I am grateful for the appreciation and compassion that I wouldn’t have without it.
Gratitude itself improves pain and accelerates healing.
The best remedy has been the (trial of the) practise of accepting and letting go. Letting go of my loss of control, my fight against the pain and my dream of a life without pain.
Letting go Non-attachment to detachment. Courage and endurance. Letting go doesn't mean ignoring or isolating, it means observing, reflecting and acting. Actions in the form of mindful practices of compassion and gratitude. No answers, no patterns, no control, only nature. Upeksa in Buddhism, equanimity, might what letting go floats you to. You will see with understanding. From within the network of everything. Breathe in, let go, breathe out. Expectationlessness. Openness. Emptiness. Only let never go of your values.
Sometimes there is no direct explanation for the pain felt and I am aware of it, so it does exist although it doesn’t (Mona Awad’s book All’s Well comes close to it: black humor, realistic, Shakespeare, chronic pain, suffering, theatre, dream vs reality and more; suffering is turned into a beatiful gift here.). Not everything needs to be understood.
I do affect a sorrow, but I have it too.
from All’s Well That Ends Well, W. Shakespeare
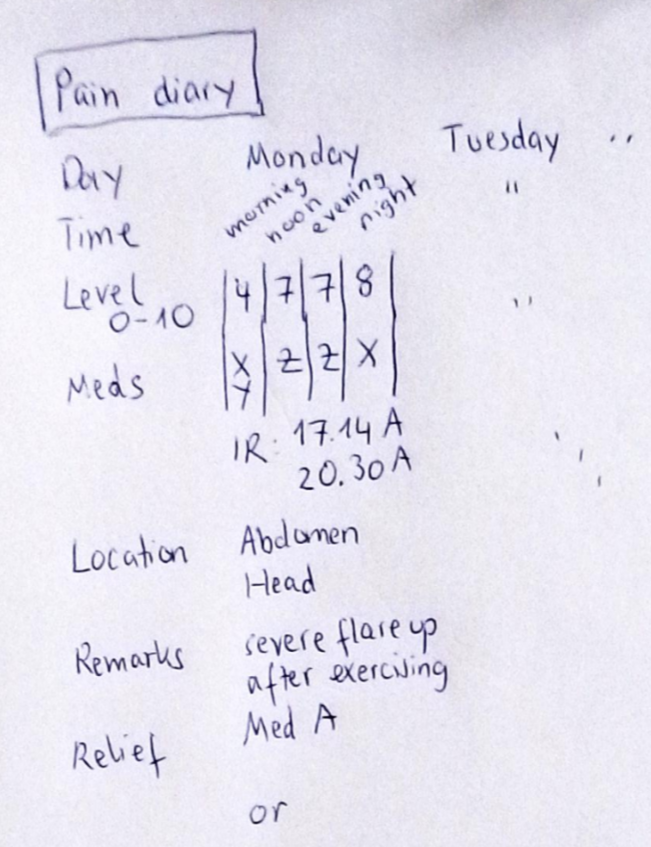
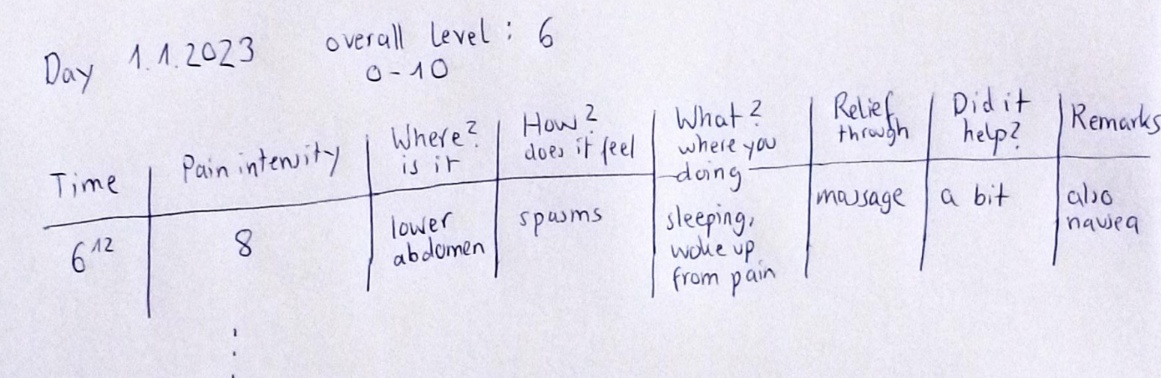
Another useful tool is a pain diary where you write down everything that belongs to your pain: intensity, quality, dynamic throughout the day, things that improve or trigger it, list current measurements and their effects etc. When you look back you can see whether things had a positive or negative effect. Sometimes progression can be very slow and you won’t notice it otherwise or seemingly unnoticed factors might have an effect.
… CIPO Pain
Ideally, such an extreme motility disorder should be treated without motility decreasing meds (which are opioids – most often the most effective ones, antidepressants, anticonvulsants). The first approach should be non-pharmacological as described earlier: abdominal massage, TENS, mobility, cognitive and psychological therapy etc. Additionally, motility stimulating treatments (see here) can improve the underlying problem and its pain (from stagnation of fluids, stool), too. Dilatation and distention caused pain may be softened by drugs that improve gas absorption or by decompression measurements (rectum splint, tubes for drainage, temporary or long-term; ostomies).
However, usually patients need treatment beyond. A combination of non-opioids, opioids, and antidepressants (e.g. Mirtazapine which also helps with nausea) in low doses is often used. If the patient suffers from CIPO due to an autoimmune issue, immunosuppressive therapy can also improve the pain level.
Methadone has been a more favourite choice for long-term opioid therapy due to weaker side effects of slowing down motility and addiction.
Frequent meetings and follow ups with the interdisciplinary team of pain experts and gastroenterologists are needed. Ideally, the patient shouldn’t be on any meds that slow motility long-term. If this isn’t possible, counterbalancing drugs should be administered, for example, Moventik which reduces the motility decreasing effect of opioids.
On the other hand, relieved pain (improved mobility, increased happiness & motivation etc) can also improve GI motility. Hence, the right balance has to be found. Nonetheless, pain management in CIPO is very difficult and complex and often patients have severe chronic pain and/or episodes with severest pain. Along with the other symptoms our quality of life is very bad. Hence, in my opinion, one should at least improve what can be improved – even of it consists of opioid treatment.
Abdominal massage has helped me in the past years to feel more comfortable. It might not take the flare ups away, but can help with bloating and even motility. The massage mimics the natural movements of the intestines, it stimulates peristalsis. Lay down and find a comfotable position without any tension in the abdomen. Firstly, wake up the intestines by knucking or tipping your fingers on your belly and do circular, clockwise movements around your belly button. Do small circular movements (clock-wise, just like the colon moves). Start at the lower right (where stool goes from the small intestine into the colon) and follow the path of the colon up to the right flexure (just below the ribs), along the transverse colon to the left flexure. At these points do the circular movements with more pressure and longer. Then follow the colon again up to the rectum where your left pelvis is. It can mechanically push forward stool and gas. Stats show that it helps with chronic constipation, pelvic floor dysfunction and visceral hypersensitivity. You can practise it every day, for example, when waking up.
Visceral pain is very difficult to describe, since it is deep inside and so is its cause. And if you are not used to it, it can be very scary. Sometimes I feel as if my intestines strangle themselves (they actually do because of the pseudo-obstructions), they twist inside me like a very angry monster crawling through my inner body, a monster that cannot escape. Sometimes I wish I could take my intestines and throw them far away. Extreme cramping, colics and dilatation that make me unable to breathe or move or speak or think. Everyone who has had an ileus knows that this kind of pain is one of the worst. Now imagine that you have to carry at least 30% of it with you throughout the day with several episodes of 90%s daily. It is horrible. CIPO pain is throughout the abdomen, from the pelvis to the chest, and the dilated intestines also push against the back causing tremendous back pain which leaves me unable to stand or sit. In flare ups I can only lay down in fetus position and wait until it subsides. There is a deep pressure inside me. In enteric neuropathies the intestines often show irregular movements, for- and backward, sometimes strong constractions, sometimes none…it is completely unpredictable. The pain improves, no movement at all, nausea starts and I wait for the vomiting. It is an endless cycle of pain, nausea, pain, nausea, pain, vomiting… Sometimes the pain feels so unnatural and so distant that it can only be depicted by my groans, cries or screams; the absence of words and eyes that tell: ‘ I cannot go on anymore.’
Despite the fact that CIPO often affects the whole GI tract, localised visceral pain can occur. Either from a local issue (such as a local pseudo-obstruction) or from referred pain. Here pain is felt in an area where the pain is referred to i.e. not where nociception or damage necessarily occurs. For example, pancreatitis typically causes back pain. And so does severe bloating/dilatation of the intestines in CIPO. In my case I feel extreme pain behind my ileostomy where stagnation of fluids and air causes pressure. It doesn’t make any sense, however, that I only have those specific pain spikes only behind the ileostomy. A book example for referred pain (or radiating pain as I still feel pain in my whole abdomen, too) – unfortunately, it doesn’t help in its management. The exact mechanism isn’t known yet, but probably there is some ‘confusion’ going on during the evaluation of signals (either of layers e.g. skin irritation is confused with some deep tissue damage or of areas e.g. in the same spinal segments that are swapped).
Langston Hughes
Hold fast to dreams,
For if dreams die
Life is a broken-winged bird,
That cannot fly.
Philosophy of Pain
From the earliest beginnings, one of the major debates has been: Is pain emotion or sensation? Or both?
Aristotle argued that the dynamics of pleasure and pain are involved in all emotions and behaviours. Our associations to pain or pleasure directs our behaviour toward or away from objects, hence, causes all movement. Additionally, it creates and shapes our character from our actions, since what we link to pain or pleasure tells us what to do and what to avoid. According to his philosophy, a virtuous (wo)man is someone whose pain and pleasure associations lead to virtuous action. The Greek saw emotional and physical pain as one identity, because they were caused by the same.
Later Descartes introduced the ‘brain’ part of pain (obviously, as presenter of the Renaissance), basically a dualism inside his cartesian dualism. He tried to explain how pain perception arises from the interaction of body and soul. Phantom pain must be caused in the brain, since no limb can cause it anymore; he concluded: pain arises in/from the brain.
For Bentham, pain was almost totally objective (he even based his theory on utilitarianism on it). Pain and pleasure are both the final cause and main motivation of one’s actions.
Keats was one of the first who concluded that pain is a necessary part of life. It is the bridge that supports us through the gap of knowledge, because suffering and pain raises many questions about ourselves and life itself. Finding these important answers can be seen as a sense of life. Many of his poems (see, for example, ‘Ode on Melancholy’) have pain and suffering as a theme, you can feel that he used poetry as a personal way of escape and remedy (he suffered from chronic pain himself). ‘Do you not see how necessary a world of pains and troubles is to school an intelligence and make it a soul?’ Pain brings knowledge, knowledge about life and all its beauty. We should embrace our pain, it flourishes our soul. Our sadness or suffering should be combated with our natural beauty. Pain and pleasure are inevitably linked.
(…)
She dwells with Beauty—Beauty that must die;
Ode on Melancholy, J. Keats
Later, Intensity theory shifted the focus back towards our emotions: pain is the emotional reaction towards certain stimuli which are above a threshold. Specificity theory pointed out that pain is isolated from all other senses.
In the end, cartesian theory dominated (also the Western pain management approaches) until Gate theory was developed when the medical sciences embraced after the second World War: pain is processed in the brain/from the central nervous system only when a signal arrives through a gate between brain and where the stimulus is from. Our emotions and other factors can make it easier or more difficult to open this gate.
The biopsychosocial model, mentioned above, is the main theory today.
For Nietzsche, humans are built of two parts, a creative part and a part that is created: mind and body. Our body inevitably suffers and the mind has to make something new and beautiful out of it. In his opinion, suffering is in fact the only way to put value in life as from suffering arises enhancement and growth. Pain makes us stronger.
Hence, pain itself should be valued, because it makes life more meaningful and it is an opportunity to develop character through self-knowledge, awareness and creativity.
Pain helps us to look deeper into our body, our body’s nature and sensations and, thus, improves the understanding of our bodies and our feelings.
I think Nietsche’s view is very optimistic and we should learn from it. We shouldn’t be afraid of pain. As Nietzsche said:
Only great pain, the long, slow pain that takes its time… compels us to descend to our ultimate depths… I doubt that such pain makes us “better”; but I know it makes us more profound… In the end, lest what is most important remain unsaid: from such abysses, from such severe sickness, one returns newborn, having shed one’s skin… with merrier senses, with a second dangerous innocence in joy, more childlike and yet a hundred times subtler than one has ever been before.
Friedrich Nietzsche, The Gay Science (sometimes also The Joyful Wisdom)
In ‘Beyond Good and Evil’ it becomes clear that pain is something necessary and, in fact, a good thing, it is an amazing teacher.
Suffering is not an evil in itself; it becomes evil only when it is not endured consciously or when it exceeds our capacities for comprehension or endurance.
But how to endure it? We should use our knowledge, our ratio and sensing, which all amplify our awareness.
However, I don’t fully agree with him, it doesn’t necessarily make us stronger. It can definitely drain us, physically and emotionally. So much that we cannot escape from it anymore and cannot grow from it. A life with severe chronic pain and endless (emergency) interventions; a terminal illness that restricts almost all opportunities, leaves little space for development or sources of creativity and such. There is only a certain amount of space that can be filled with pain and suffering. Growth needs space.
Nonetheless, we can endure it – as long as we find some sense in it. Meaningless suffering? Does it even exist?
Schopenhauer had a rather different approach, he expressed that consciousness amplifies the pain (of life), but has no effect on pleasure. In fact, he had a rather pessimistic view where he depicted the ‘futility, uselessness, and pointlessness of our lives, in which there is nothing but suffering, frustrations, and pain’ in his essays e.g. On The Vanity and Suffering of Life. He argued that we will never be content – even when our dreams come true, we finally regret their loss. How can we be happy in life when we suffer? Schopenhauer would reply: We should not expect to be happy. Nonetheless, Schopenhauer concludes that he doesn’t know anything else that is more absurd than our negative attitude towards pain and suffering.
Again, his view is quite similar to Buddhism’s philosophy where we should stop pursuing our satisfactions only to be discontent from this endless, impossible struggle. On our path to the end of suffering we should let go of our desires (and our non-acceptance). Schopenhauer also had quite a Buddhist aproach in his moral of compassion********. For both, Nietzsche and Schopenhauer, suffering was an/the integral part in their philosophies.
Kathy Charmaz (developer of Constructivist Grounded Theory*********, a major research method in qualitative research) depicts another interesting view on pain, for example in ‘Loss of self: a fundamental form of suffering in the chronically ill’ and in her dissertation ‘Time and identity- the shaping of selves of the chronically ill’. She emphasises that the combination of physical pain, the following psychological distress and the effects of medical interventions cause us patients to suffer and that the awareness and knowledge of the underlying chronic conditions play a major role. The loss of self in the chronically ill and the fear of it are equally difficult to manage as the pain itself. Illness and pain eradicates our former self-images and often there is only little space to create equally new ones.
She mentioned four main aspects of suffering:
- leading restricted lives
- experiencing social isolation
- being discredited
- burdening others
Loss of control over health, the body and its sensations. Loss of perspective, possibilities in life, manageable activities and realistic goals. All of that leads to loss of a valued self-representation or provides fewer opportunities to construct a new self.
For me, she raises a very interesting point: the relationships between suffering and the self. Where compassion also arises from. Hence, there is an ill nature of compassion development from the pain and it is a/the major task to escape from this circle.
Later, Charmaz and Rosenfeld, continue their evaluation and also add the issues of the visibility and invisibility in chronic illness and disability.
Chronic pain patients become dependent and immobilised. They do not only lose their self-esteem, but in the following (if no counter action is present) even their self-identity. However, no possible actions are suggested.
The universal suffering called Dukkha in Buddhism refers exactly to this issue of loss to find one self as our desires aren’t fulfilled. Where Buddhism recommends letting go of them at all. Enlightenment doesn’t mean anything else than the realisation that ‘the self’ does not exist.
The philosophy of pain influenced the general perception of pain and, thus, the general approach of pain management throughout history.
Life isn’t suffering. Suffering is an inevitable and integral part of life. Always remember it.

Small Fibre Neuropathy
Talking of pain, I wanted to give a brief explanation of the recently mentioned SFN, Small Fibre Neuropathy.
SFN affects the smallest fibres of our nervous system, it involves A-delta and C nerve fibres (see above), probably due to distal loss of axons and/or neuronal degeneration.
Typical symptoms include burning pain in the extremities (hands and feet) and numbness – but not only (!). There is a variety of symptoms that are different in the individual patient. It might affect sensory and autonomic fibres, followed by sensory issues and/or autonomic dysfunction (see last posts about autonomic neuropathy): GI, bladder function, cardiovascular issue e.g. POTS and orthostatic intolerance, thermoregulation, sweating…and also pain related to thermal and mechanical stimuli.
Thus, SFN often comes with many other diagnoses such as dysmotility, MCAS, autonomic neuropathy etc. Usually, one cannot tell which condition is primary and which is secondary.
SFN can be idiopathic, hereditary (see SFN genes, Morbus Fabry) or because of metabolic (common: diabetes, severe or long-term lack of vitamin Bs) or immune-mediated (e.g. rheuma) conditions, infections (e.g. HIV) or after chemotherapy and other toxic issues.
One differentiates between length-dependent or non-dependent forms. The former starts in the periphery and may affect large fibres later. An early diagnosis might help in reducing its progression and pain involvement. In length independent forms patients might suffer from untypical symptoms (e.g. GI issues) first followed by issues in the extremities years later.
Unfortunately, diagnosis is often after many years in which patients have already collected many other (mis)diagnoses and/or the illness has already progressed beyond a treatable limit. Typical tests for SFN include QST (analysis of reaction to stimuli), QSART (assessment how much sweat can be produced), autonomic testing (such as tilt table test) and finally a skin biopsy (where pathology should confirm a reduction of small nerve fibres, a so called reduced intraepidermal nerve fibre density).
SFN can be treated when the underlying condition can be treated. Further diagnostics such as full blood count, Diabetes testing and/or genetic testing etc is needed. Vitamin deficiency needs supplements, the nerve fibres can recover and so does the condition. Immune-mediated conditions might benefit from immunosuppressive therapy such as Ivig (Iv Immunoglobulins) and Diabetes induced nerve loss can be counteracted with drugs and Diabetes control, weight management and exercises.
If it is idiopathic or the underlying illness cannot be treated or found, only symptom management is left. Autonomic issues have to be treated accordingly e.g. orthostatic intolerance with meds or manoeuvres; pain management (for neuropathic pain: include anticonvulsants, antidepressants, topical anaesthetics, narcotics and non-pharmacologic treatments e.g. heat/cold, massage, TENS, neuromodulation), GI issues according to their manifestations (see dysmotility measurements). Unfortunately, a majority of patients suffer from severe chronic pain that needs multidiscipilinary treatment.
And Finally…Top Gadgets for Chronic Pain
…aka the best gift ideas for chronic pain friends. Here are some top gadgets for chronic pain from my own experience (hence, mainly for abdominal pain).
- Hot water bottle, electric warmer, heating pads / cold packs; fango (ideally something that is flexible)
- Oil (such as mint oil against headaches, clove and black cumin oil for abdominal massage)
- Pill box (pain meds always nearby, also when somewhere else)
- Distraction: books, magazines, riddles, audiobooks, movies (series, Netflix and so on)
- Fascia roll, foam roller (hedgehog ball, thera cane… for myofascial pain, to soften trigger points)
- Thera band for a broad range of exercises for all muscle groups without any other tools
- TENS unit (some insurances cover it, give it a try)
- Pillows (probably an own post :’) – the RIGHT pillows to reduce neck stifness, keep a pillow between or under your legs to reduce abdominal tension)
- Scents (to get you in a better/calmer mood, but also against nausea: citrus aroma oil) candels, aroma oil etc
- Shower bench (especially when he/she suffers from autonomic neuropathy/orthostatic intolerance etc)
- Loose trousers/leggings (for bloating, ostomies and co)
- Tiger balm or similar for rubbing against muscular pain
- (Compressing) braces for joint issues
- Compression gloves, ‘Taschenwärmer’ etc for Raynaud people or Frostbeulen
- Anything that makes him/her happy (distraction, focus, anything else than pain)
- Infrared light
- …

Recommendations
Two songs
Number 1: Asaf Avidan, ‘Turn of the Tides under the Northern Lights’
The sun, it rises and sets
My homeward path is the place where it rests
The love for life will always take us home and suffering ceases. Dream and believe…
It isn’t easy to keep the balance between healthy hope, realistic optimism and the frustration (?) following inevitable drawbacks and disappointments.
We shouldn’t get lost in our dreams. However, without some dreaming and believing I would not be here right now.
I believe in my powers and the personal and medical support. I believe in my endurance, persistence and love for life. I believe in my purpose and effort. I don’t chase my dreams I had back then, I am not a fool. But I do chase my dream of some health improvement or at least a more stabilised health.
As a scientist, should I believe (in) something until the impossible is proven? And as a human being?
What holds us back? The fear of failure? The expectations? The memories and past experiences?
Number 2: Bob Dylan, ‘Chimes of Freedom’
(…)
As we listened one last time an’ we watched with one last look
Spellbound an’ swallowed ’til the tolling ended
Tolling for the aching ones whose wounds cannot be nursed
For the countless confused, accused, misused, strung-out ones an’ worse
An’ for every hung-up person in the whole wide universe
An’ we gazed upon the chimes of freedom flashing
This song from 1964 is about the freedom we all wish we had. But we won’t ever have. You may interpret it as political liberty (Kennedy, Civil Rights Movement) or my own personal freedom. The freedom we cannot receive and causes so much pain and suffering. Well, not the freedom itself, but our longing towards it. Isn’t it bittersweet? As if the singer is about to realise how much inevitable pain and suffering there is. The real freedom of every individual, the freedom that we (want to) meet every day, not the one philosophers discuss about.
Just like the singer finds shelter from the thunderstorm we all feel safe somewhere. We should be grateful. The storm is too strong to be fought. As the singer has to accept it, we have to accept the painful conditions of life. We have to live WITH them, adapt, use them to create something new rather than lose our strength in an impossible fight. There are powers much higher than we may anticipate or imagine, conditions we cannot change, but we can only live through.
When they shelter, reflection begins. Only when painful things happen towards us, we halt in and start to see clearly. Reflection, awareness and gratitude (for what has been, was or is) should’t only start in such moments.
Moreover, when watching the storm the singer thinks of all people, not only himself. As I have already mentioned before, we should face pain as a community. Happiness and pain can both be equally shared. Together we can manage the most painful phases of life.
Things can change. Change of the intolerable is not impossible.
The love for liberty will win.
Through suffering and uncertainty.
and more.
Film: Il signor Rossi cerca la felicità
Questa è la felicità
Chi la cerca già ce lha
Questa è la felicità
Mr Rossi looks for happiness, theme song
‘This is happiness/ Those looking for it already have it/ This is happiness’
After some short movies between 1960 and 1974, the animated movie ‘Mr Rossi looks for happiness’ was produced by Bruno Bozzetto. His movies are of political/satirical nature, he also created ‘Allegro non troppo’ which I still haven’t really understood. Anyway, I would like to recommend Signor Rossi – we can learn a lot from this movie.
Rossi (Rossi is the most common surname in Italy – a man like you and me) lives and endures a life without happiness. He works in a factory led by a bullying boss whose home is next to his, he feels alone in the crowd on the way to work where he monotonously does the same movements every single day…
But wonders happen, one day a good fairy gives him a magic whistle with which he can float through spacetime in order to find his happiness (?). Gaston (the dog of the boss who can talk after the fairy experience) accompanies him and they become good friends.
They need to tackle obstacles in which the boss basically appears as the antagonist through the times (Stone Age and ancient Rome, Middle Ages and pirates, fairytale world and ancient Egypt, Wild West and in the future).
Spoiler ahead
In the end, they reach the present without apparent change until the boss blows the whistle himself and disappears in the present. Happiness develops on their journey, friendships like the one between Rossi and Gaston are far more important than any wealth. Happiness is right at his home (along with some little changes and disappearances of things that are not good for him).
Isn’t this a cute story?
Many times in life we find ourselves back where we started. No direct improvement, but with a collection of so many new perspectives, opinions and special views on life.
Moreover, it doesn’t matter where we go or escape to – our fears and problems won’t be left behind us. We take them with us, wherever we go. Hence, we have to face them. Better sooner, than later. Life isn’t easy and we shouldn’t watch out for simple life.
The music was written by Franco Godi who also made the music in La cabina.
‘Happiness is a process and happiness is the path.’ Camus would have said.

More recommendations in philosophy thoughts are soon to be posted. I have also updated some of the pages e.g. regarding TPN and dysmotility (mainly about the enteric nervous system and the risks and benefits of TPN).
With chronic pain comes uncertainty. More about compassion, uncertainty and how to deal with it as well as autonomic neuropathy, over-therapy vs neglience as well as palliative care and loved ones as carers can be found in the next posts.

* from Pali, suffering in the sense of uncomfortability or discontent or unsatisfactoriness, internally created.
** Impermanence is probably THE cornerstone in Buddhism. It reminds us of the inevitable change of everything. Everything will vanish at one point. Impermanence is basically time, we cannot escape from it. Its consequences we have to accept which causes the pain we have to deal with. To understand it fully, we do have to follow the whole Buddhist path of course. In my eyes, impermanence emphasises the beauty of life.
*** The difference between mindfulness and awareness in Buddhism is important to understand. Mindfulness arises from the state where our thoughts are acknowledged without judgement or hard concentration. Mindfulness can not only be practised during meditation, but also at every moment throughout the day, during walking or eating or any other actions. Mindfulness arises from the present moment and goes hand in hand with appreciation. Consciously, we are present in the specific moment. Awareness, however, can be seen as something complementary that helps us to RETURN back to our state of mindfulness e.g. when our thoughts wander off during meditation, judgement disturbs the peacefulness, our awareness can take us back. Hence, awareness needs some broader understanding into your environment also. Basically, awareness makes mindfulness possible which again is taking us back to our consciousness, the most natural state. Hence, mindfulness and awareness should work together and are the foundation for meditation.
**** IASP stands for ‘International Association for the Study of Pain’. They promote research, education and policies for the general understanding, prevention and treatment of pain, especially chronic pain. Collaborations of scientists, doctors, health care providers and further disciplines try together to improve pain relief and its access and resources worldwide. Education for the general public is as important as the individual teaching of patients, their carers and loved ones. See more about definitions, guidelines, recommendations, further pain organisations etc here. PAIN is its own journal and covers all kinds of pain subjects, mechanism and treatment of pain including recent updates.
***** There are imaging studies (functional MRI, PET etc) that show that noxious stimulus and pain are dissociable at the level of brain activity. Moreover, chronic pain alters brain structure e.g. gray matter and thickens the cortex. However, so far research doesn’t know how to colerate these alterations with pain conditions nor how to develop more efficient treatment options from it.
****** Pain and suffering (beyond Buddhism):
In my opinion, suffering is an ‘overall’ attitude, whereas pain is a sensation located somewhere in the body. Pain is non-intentional, suffering is intentional. I am in pain and I decide that it lets me suffer, suffering is the individual interpretation. Suffering does not always arise from pain, but pain usually causes some kind of suffering (not for the enlightened Buddha). Pain leaves more options. Suffering is more on an existential level, it changes our character, it forces us to adapt our style of life, ambitions and personality. It is caused by our non-acceptance of something that has occurred or happened to us. Thus, accepting the condition, the suffering and all its components, your emotions, is vital in the reduction of suffering.
Suffering is always a secondary process (pain, for example, can be initial).
Even in pain I can smile, I can find joy. But when I truly suffer, it is very difficult to see beauty around me. Suffering and hopelessness catalyse each other.
Pain and suffering can occur intertwined, dependent or independent from each other.
In medicine, we look for better pain management and not for the improvement of suffering.
Both are essential and inevitable. However, only up to a certain threshold. Practice mindfulness, (self-)compassion and (self-)kindness to deal with any imbalance.
In my opinion, suffering is pain amplified by non-acceptance. And pure acceptance can be taught and learnt.
Often, we associate emotional discomfort with suffering, physical one with pain (any definitions aside), probably because we classify our soul above our body, so do we understand suffering above pain.
Compassion alleviates suffering. Through practice we can improve our empathy towards others, but also the understanding of our own feelings. Along with that, we can spread kindness to others and ourselves, be gentle and comfortable to our environment and our own body and mind.
Tips to practise self-compassion:
- Allow yourself to come close to your emotions.
- Be aware of them. Analyse them. Their cause, intensity, intent, quality…
- Accept them.
- Be as gentle to yourself as you are to your loved ones.
- Through mindful thoughts and actions, deep breathing, meditation, smooth movements…
- And gratitude for your body which can do all of that and your mind that can support your body and beyond.
- Understand yourself as a single knot in the net of all beings.
- Analyse your situation in RELATION to your environment. What are the causes and conditions that took you there and what effect do your thoughts and actions have on you and your environment?
- Put self-judgement aside.
- Practise it as much as possible. Self-compassion is learnable.
- Practise self-care, too. Balance social support and interactions with isolation, thoughts and actions with yourself alone: Go on walks, write down your own thoughts for yourself only, cook yourself a meal…
A good trick is to picture someone else in your situation. How would you feel about it? Now give yourself the same amount of compassion and kindness.
It is self-compassion, not self-esteem or self-criticism that improves suffering.
More resources on how to accumulate (self-)compassion can be found here (‘The Compassionate Mind Foundation promotes an evolutionary and bio-psycho-social informed approach to compassion’).

******* Pharmacological options
In pain management there are six different categories of schemes
- Narcotics/opioids and local anaesthetics for severe chronic, acute, post-op, cancer pain
- NSAIDs for mild pain (ideally not long-term)
- Muscle relaxants for cramping, muscle spasm type pain
- Anticonvulsants for neuropathic pain
- Antidepressants for nerve damage, additionally in chronic pain management
- Selective norepinephrine reuptake inhibitors (SNRIs) for neuropathic pain, depression (as consequence of chronic pain)
And obviously all kinds of meds that might improve the underlying illness and, hence, the pain (e.g. immunosuppressive therapies in autoimmune illnesses).
The named drugs (according to the above mentioned WHO guidelines) can be given in the following forms:
- Per os, orally: liquids, pills,
- Through the mucosa: sublingual pills, spray
- Transdermal: patches, spray
- Parenteral: subcutaneous ‘sc’, intravenous ‘iv’
In pain management, often one tries to have a continuous level of the medication for the constant pain level and (if needed) immediate release ‘IR’ options for breakthrough pain (i.e. increased pain episodes in flare ups). For example, retard pills twice a day and when there are still spikes IR pills (often sublingual as the absorption is faster here). When patients suffer from malabsorption or other issues that make oral intake difficult, one prefers the other paths. Opioid patches that need change every few days are often given to elderly patients that might forget the intake of pills. Transdermal (through the skin) patches are also a good option in malabsorption patients without iv access. Sublingual means ‘under the tongue’, the drug is absorbed through its tissue and then forwarded to the cardiovascular system.
For subcutaneous application one needs to inject the drug into the subcutaneous fat tissue; for ivs the patient has to have an iv access, either temporary (e.g. in the clinic after surgery) or long-term (port catheter, see my other posts). In the latter case patients carry a pain pump with them. Some drugs are also injected into the muscle tissue (intramuscular).
Parenteral, especially iv, application has the fastest action and as it is directly given into the bloodstream, fully absorbed.
An iv pain pump can give a continuous amount throughput the day to reduce the overall level of pain, but one can install a bolus function where the patient can ask for an additional bolus when spikes occur (often patients can administer it themselves, ‘PCA’, according to a programmed plan of the pump e.g. with a time interval between boli or a maximal dose per day).
When chronic pain patients need long term opioid treatment (beyond a certain dose per day) one should discuss the option of invasive procedures such as
- nerve blocks, temporary or long-term
- intrathecal pain pump
An intrathecal pain pump is surgically implanted and gives tiny amounts of opioid (at the moment, there is only morphine and an antispasmodic approven) into the spinal cord. Thus, the amount needed for the same pain level is a lot less than with the other paths. The drug is given exactly where the pain processing takes place. (If we take pain meds, they work everywhere – not only where the pain is located). The reduced amounts mean reduced side effects, but the surgical implantation and maintenance have risks as well (catheter moving, infection, meningitis, skin irritation, wounds etc since the whole pump has to be implanted inside the fat tissue).
Pharmacological treatment should always be administered according to a plan and under professional supervision (drug interactions, reactions, allergies, possible contraindications, individual dosage, slow introduction and withdrawal etc). Pain is a dynamic process, the plan has to change according to it.
******** The Mitleid/compassion moral by Schopenhauer was criticised by Nietzsche. But I think that Nietzsche referred to Mitleid as pity not compassion (unfortunately, in German we only have one word for both). Schopenhauer definitely talked about compassion, the desire of someone else’s well being – one of the four motives (Triebfelder), the motive for worthy actions and purely altruistic. Interestingly, he concluded that Mitleid arises only when people feel similar to the ones to whom they grow compassion to. Nietzsche raised the issue whether Mitleid then arises from the other person’s suffering and that the desire for one’s own end of suffering grows into ‘compassion’ or rather pity. I think this is quite an interesting starting point for debate.
********* Grounded theory means ‘systematic methodology that involves the construction of hypotheses and theories through the collecting and analysis of data’, see also Glaser & Strauss. For chronic illness research and grounded theory, see also ‘Good Days, Bad Days: The Self in Chronic Illness and Time’ (1991)
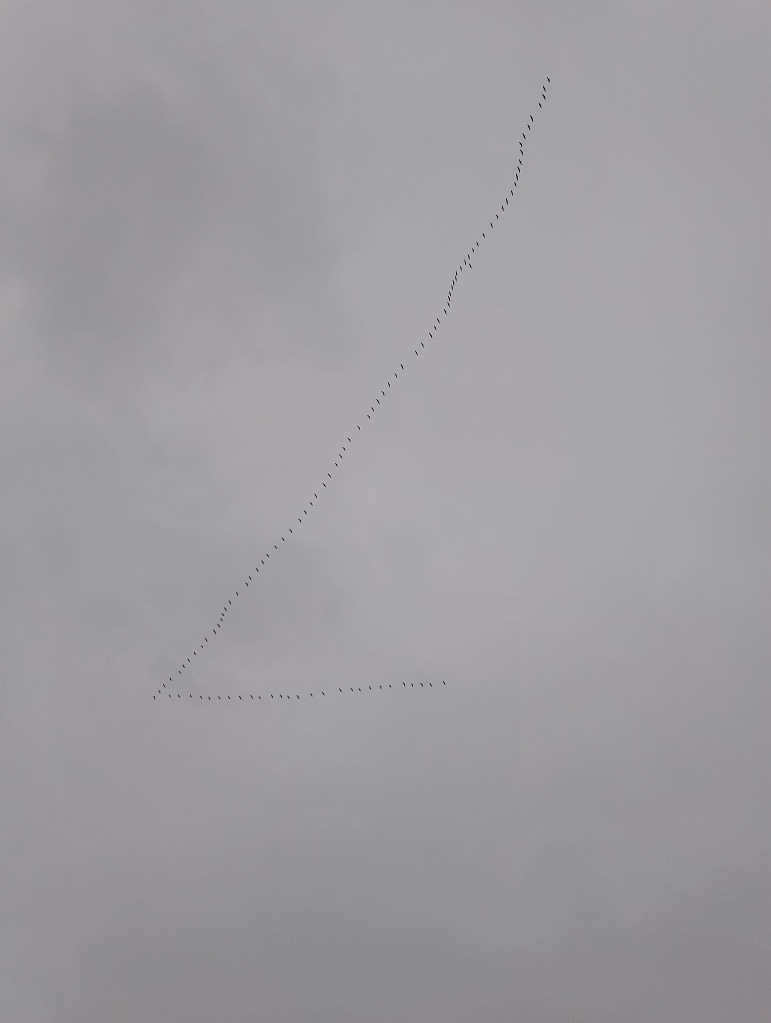


3 thoughts on “In the Rain (Reign) of Pain”