In the following I would like to give some information on CIPO (chronic intestinal pseudo-obstruction) as an example for the probably severest motility disorder, its diagnosis and treatment. Obviously, a large part can also be applied to other conditions* that I will cover later on.

Motility is the ability of the GUT to move, doing the peristalsis – how it pushes forward food and air and its digestion. As described in this post, it is mostly dependent on the enteric nervous system i.e. the autonomic one which acts independently from our brain. The exact processes are quite complex and still not fully understood.
What is it?
I would classify it as the severest motility disorder. The patient’s nerves and/or muscles in the intestinal tract don’t work properly or lost their function such that stool/fluid and air cannot be transported forward. The GUT doesn’t show any peristalsis (at least not a working one). Usually it is defined for the smaller and larger bowel, but some patients also suffer from gastroparesis (slow/no emptying of the stomach) and problems with swallowing due to dysmotility in the oesophagus, some also have problems emptying the bladder (both bowel and bladder/ureter are smooth muscle cells). It is called chronic as often they are born with or acquire it by a late onset of illness or events (see causes for primary and secondary ones) and it cannot be cured. There is also an acute version for colonic atony, ACPO (acute colonic pseudo-obstruction), also known as Ogilvie’s syndrome**. With pseudo-obstruction we mean that the intestines behave as if there was an obstruction somewhere, but images don’t reveal any mechanical issue such as adhesions or a tumor. Symptoms and first findings still indicate an obstruction, the intestines are hugely dilated and filled with air and fluids.
Symptoms?
Abdominal distention, lack of peristalsis i.e. severe constipation up to (sub)ileus symptoms (abdominal cramping, nausea, vomiting up to stool vomiting, early satiety, inability to pass gas, severe bloating,… an acute ileus also causes fever and I actually had severe back pain before anything else), abdominal pain (often visceral hypersensitivity comes along with Cipo), distention, nausea, vomiting, weight loss up to severe malnutrition and cachexia, early satiety, trouble swallowing, urine retention or incontinence – depending on which organs are affected. Secondary issues due to the dysmotility accumulate: SIBO, leaky gut, perforation, symptoms from the lack of certain vitamins and electrolytes or micronutrients***, malabsorption …
Causes?
If you are born with it, CIPO is primary. Often it is a secondary condition from other conditions such as IBDs that put the GI tract under stress or EDS and other connective tissue diseases (lupus, scleroderma) since supporting structures don’t work due to the defect in collagen. The decrease or absence of the connective tissue in the region where the myenteric plexus works and in the muscle layers itself has been investigated as causes for colonic dysmotility. Other primary illnesses are the ones that affect the nerves and muscles such as Parkinson’s or Diabetes as well as mitochondrial illnesses (where mitochondria don’t ‘produce’ enough energy resulting in muscular dystrophy). There are single cases of many other health conditions, but also patients that develop CIPO after ‘sudden’ events such as infections e.g. Chagas or after abdominal/pelvic surgery and spinal cord injury. Further, it can be caused by damage of the brain-gut connection e.g. after a stroke. Often the cause is not known, which makes treatment of this complex condition even more difficult. It is also a rare disease and due to its distinguished origin as primary or secondary cause there is no general ‘recipe’ one might follow for treatment and diagnosis. Nonetheless, it is mostly caused by abnormalities of the enteric neuro-musculature and/or its autonomic innervation. Primary mutations can be classified in myopathies and neuropathies as well. Former manifest in rather diffuse abnormalities in the muscular layers and latter as degeneration of nerves and dysplasia of the ENS. Common ones are megacystis–microcolon–intestinal hypoperistalsis syndrome (MMIHS) caused by a ACTG2 mutation, mitochondrial myopathies (e.g. mitochondrial neurogastrointestinal encephalomyopathy, MNGIE, due to a mutation in the TYMP gene) and the chronic atrial and intestinal dysrhythmia syndrome (CAID) where the SGOL1 gene is mutated. Some doctors mention a third class, mesenchymopathies, which include abnormalities of the interstitial cells of Cajal (pacemaker cells in the gut muscles) and also result in bladder problems due to abnormalities in the muscularis propria (deep muscle layer of the bladder). Obviously, it can also be a mixture of the just mentioned ones. Following the nerves as primary cause, Cipo is often accompanied by dysautonomia (ANS isn’t working properly) or autonomic failure (ANS is damaged, does not work). Symptoms range from POTS, IBS, orthostatic intolerance, loss of sweating etc with autonomic failure being more severe and a constant issue. Latter, as a primary cause for Cipo, can be classified into degenerative (Parkinson’s …), some (probably) autoimmune (acute acquired, cancer…) and metabolic (diabetes…) disorders. It is a chicken-egg problem to find out whether dysautonomia causes gastro problems or the other way around.
Diagnostics?
One should find a good and specialised (neuro)gastroenterologist who works in an interdisciplinary team depending on the cause and symptoms. Often Cipo prominently manifests in x-ray images where you can see the typical dilatation of the intestines corresponding to a severely swollen abdomen. Next, one should confirm lack of mechanical obstruction via an ultrasound and MRI (ideally Sellink type where you drink a contrast agent that fills the bowel loops such that one can see any abnormalities, obstructions, inflammations etc on the images) or other causes of intestinal atony e.g. due to the lack of blood flow via a CT or duplex ultrasound (ischemia). Then, colonoscopy and endoscopy may be carried out to see whether more organs are affected or how they are by Cipo, any secondary issues such as inflammations, biopsies etc. Cipo can be fully diagnosed in motility measurements via manometries (endoscopic measurements where intraluminal pressure sensors inside the catheter used via NJ tubes for the smaller bowel and colo tubes for the larger bowel measure the exact patterns of all contraction events – also important to differ between enteric neuropathy or myopathy, if the manometries are positive, but radiological findings don’t really show Cipo patients are often diagnosed with enteric dysmotility) before and after food intake as well as administration of motility increasing meds and transit tests (measurements of the duration of the movements through the gut). Latter can be pills (Hinton test)/sitzmark study that you take for one week which dissolve in many beads inside the intestines. The doctors can then calculate the transit time of the bowel as the x-ray image on the last day will show how far they got through the gut. Normally, the patient should have emptied all beads via stool. In dysmotility patients, however, beads remain in the bowel e.g. for defecation disorders (malfunctioning rectum) they collect inside the rectum, for colonic inertia they distribute evenly in the larger bowel, for slow transit constipation a certain number of beads still remain in the colon, especially, in the descending bowel. This test as well as the smart pill test (where a wireless capsule measures the duration in each part of the gut via measurements of temperature, pH, pressure etc – I wouldn’t recommend using it in severe cases of dysmotility as it will obviously simply remain somewhere in the gut and won’t get out if patients aren’t able to pass any stool or gas) can also give evidence whether there are certain parts that don’t function or whether it is an overall gut problem. Further, there are special breath tests that can give some hints regarding transit time and SIBO (small intestinal bacterial overgrowth due to the chronic dysmotility) as well as intolerances which should also be excluded for gastro symptoms. Orocaecal transit (from the mouth to the colon) is measured via the increase in breath hydrogen following the degradation of ingested polysaccharides (eg. after drinking a tea with lactulose) called C13 test, fructose/lactose/sorbitol intolerances (which can lead to bloating, discomfort, nausea, abdominal pain, diarrhea) calles H2 tests. SIBO is tested via glucose which is not being absorbed in the smaller bowel, but digested by the bad bacteria. Lastly, a full thickness biopsy and other biopsies (e.g. during the endoscopies) are taken to see whether there are damaged/no nerves/less ganglia etc. Former can be done endoscopically or laparoscopically and reveal certain abnormalities in histopathology or immunochemistry in all layers of the smaller and larger bowel. There is a lot of research going on which conditions are marked by what findings and how certain types of dysmotility are related to changes in the wall, ganglia, intestinal cells of Cajal, neurons, smooth muscle cells, immune cells etc. It is a small surgery (mostly a combi of keyhole and open) that contains risks since bleeding, damage of the bowel and bowel content emptying in the cavity, so it should only be done when indicated. A full thickness resection seems to be more efficient and less risky. I would recommend getting into contact with a good neurogastro department for those tests as they all need special equipment and knowledgeable and specialised doctors.
Obviously, if the underlying condition is not known, it may (!) be useful to find it out via further tests if it improves therapy options. Tests less conducted are barium swallowing to see how quickly it moves through in real time (especially to diagnose gastroparesis). To have a quick result, emergency patients are often administered contrast agent which brings two benefits, first one can see on the x-ray images whether there is some blockage and whether the transit time is slowed down and secondly, it pushes forward the stool as immediate therapeutic measurement. Once I also had a scintigraphy test where I ate some food and drank some water with radioactive traces and images were taken directly after (for stomach emptying), over the first several hours (smaller bowel) and the following five days (larger bowel).
In dysmotility patients blood tests for nutritional status/electrolytes and the breath tests for SIBO should be done as needed to help treatment.


Summary list of tests (look further below for details):
- Blood tests, urine samples – inflammation levels, lack of vitamins or minerals, underlying condition (antibodies etc), pancreas?
- Simply look at the abdomen and listen to its sounds in all four quadrants (peristalsis, bloating, severe swelling? Difference between quadrants? Bruits?) – everybody celebrates when there are sounds after surgery indicating that there is no ileus lol
- US (duplex) of organs, motility (are the intestines moving? Back- and forward? Fluid and air levels? Stool? …), exclude any problems of abdominal vessels (ischemia)
- X-ray (mechanical cause? Blockages? Fluid and air levels? Possibly after oral contrast agent to see transit time), barium swallowing
- MRI (ideally MRI Sellink, if vascular issues need to be excluded MRA or CT, also to exclude other mechanical issues such as tumors)
- Colonoscopy (biopsy: inflammation levels)
- Endoscopy, EGD (biopsy: gluten intolerance? Dysmotility in the stomach and duodenum?)
- Barium enema (anatomic abnormality in the colon?)
- Breathing tests (for motility and intolerances): H2 tests (glucose – SIBO? lactose/fructose/sorbitol intolerance?), C13 (gastric emptying, transit mouth to colon)
- Full thickness biopsy: primary neuropathy or myopathy? Ganglia? Nerves? Smooth muscle cells? Any abnormalities? Lack of nerves?
- Smart Pill
- Hinton test/Sitzmark (transit time – colonic inertia? Only parts affected? Defecation problem?)
- Manometries: esophageal, antroduodenal (gastroparesis? Dysmotility in duodenum?) smaller, colonic (larger bowel dysmotility: slow transit, pseudo-obstruction, IBS…?) anorectal(defecation problem of the rectum? Hirschsprung?)
- Scintigraphy (gastric emptying normal? Bowel transit? Fluids and solids)
- Defecation tests: balloon expulsion, MRI, proctography, pudendal nerve terminal motor latency (damaged pelvic nerves?), EMG of the anal sphincter and pelvic floor muscles
… make yourself ready for an adventurous journey through motility testings.
Ideally, one finds the cause, whether it is primary (neuropathy/myopathy) or secondary (also neuropathy or myopathy but caused by other underlying problems e.g. neurological, connective tissue or muscular diseases). Exclude any other factors that would worsen symptoms: medications such as opioids, vascular compression syndromes, psychological conditions (such as anorexia), …
I also recommend to go through those tests if doctors may have diagnosed any compression syndrome (especially MALS or SMAS) since symptoms can be very similar and before operating on those the cause for your symptoms should be clearly identified. Any abdominal surgery is a huge invasion in the motility of your gut.
Therapy?
Might also give some advice on general dysmotility issues or IBS problems.
Ideally one finds the cause and treats it. Often it is not possible to find the cause and/or it is not possible to treat the underlying condition. Treatment is then equivalent to the adequate management of symptoms and provide adequate nutritional intake somehow possible. Further, one should treat secondary issues such as SIBO, lack of vitamins or minerals as well as electrolyte, mineral or endocrine abnormalities. Unfortunately, Cipo is often progressive and affects the whole gut at some point.
- Find alternatives, adapt the lifestyle e.g. if oral food intake is possible, changes in diet may be considered: free-from diets (depends on the individual patient), low fodmap (especially to tackle SIBO), liquid or semi-solid diet to keep stool soft and relieve the bowel… For Cipo patients the usual IBS recommendations (increase fiber content, both soluble fiber (psyllium) or insoluble fiber (bran)) do not work, one rather recommends a low fiber (and if, soluble fiber), low fat, low residue (undigested food that makes up stool: fiber, nuts, seeds, raw veggies, whole grain products etc) diet with frequent small meals. Thus, there is a huge difference between ‘normal’ constipation and underlying Cipo regarding food recommendations. If tolerated, sufficient intake can be made possible with additional high calorie drinks (see below for further information******). Colonic massages, deep breathing, biofeedback, exercises (such as pelvic floor physiotherapy) etc should be included in daily activities.
- Medication. As I explain here one uses motility increasing and stimulating meds: prokinetics**** such as prucaloprids, often linaclotide for the lower gut part and the antibiotic erythromycin for the upper. I have been on resolor which seemed to have worked in the beginning, but then lost its efficiency. Due to negative side effects many meds of this class have been taken off the market in the past years, some are only allowed in certain countries, there must be a proper indication for their prescription i.e. severe dysmotility where all other meds or treatments haven’t worked. Further, any relief from constipation, keep stool as soft as possible etc with laxatives (not as chronic med as it can make things worse plus often it does not work), meds against nausea, pain etc i.e. target daily symptoms. Meds that decrease motility such as opioids or antidepressants should be avoided where possible. This is, however, quite difficult since severe Cipo manifestations are very painful distentions of the bowel which force some patients to use opioids, the efficient antiemetic ondansetron (a serotonin antagonist i.e. it blocks certain serotonin receptors and hence the signals to the vomiting centre) causes constipation… Frequent use of antibiotics against bacterial overgrowth can damage the intestines and motility, the intestines can become used to the meds and at some point patients find themselves in a never ending vicious cycle. Inflammations in the gut should be treated properly and depending on the underlying condition an immunosuppressive therapy might bring some relief.
 When meds are not working or one needs further help, tubes can support. There is the normal feeding tube one wakes up with after a major surgery (into the stomach nasogastric, NG,) and one that ends in the jejenum, NJ, nasojejunal. Latter might be helpful to pass slow gastric emptying and should be inserted under radiology. Further, PEG (percutaneous endoscopic gastrostomy) or PEJ (percutaneous endoscopic jejunostomy) or combined and JEJ (jejunostomy) which are inserted in a minor surgery through the abdominal wall (into the stomach, beginning of the small intestine, both and middle of the small intestine, respectively). They are all used for nutrition, but also for meds and can be used for flushing and ventilation i.e. for the outflow of fluids and gas and draining and de-fluid. Nutrition can be given from simple high calorie fluids with certain formulae (e.g. with(out) fiber etc) and in the most elemental formula meaning that it can basically be absorbed by the intestine immediately.
When meds are not working or one needs further help, tubes can support. There is the normal feeding tube one wakes up with after a major surgery (into the stomach nasogastric, NG,) and one that ends in the jejenum, NJ, nasojejunal. Latter might be helpful to pass slow gastric emptying and should be inserted under radiology. Further, PEG (percutaneous endoscopic gastrostomy) or PEJ (percutaneous endoscopic jejunostomy) or combined and JEJ (jejunostomy) which are inserted in a minor surgery through the abdominal wall (into the stomach, beginning of the small intestine, both and middle of the small intestine, respectively). They are all used for nutrition, but also for meds and can be used for flushing and ventilation i.e. for the outflow of fluids and gas and draining and de-fluid. Nutrition can be given from simple high calorie fluids with certain formulae (e.g. with(out) fiber etc) and in the most elemental formula meaning that it can basically be absorbed by the intestine immediately. 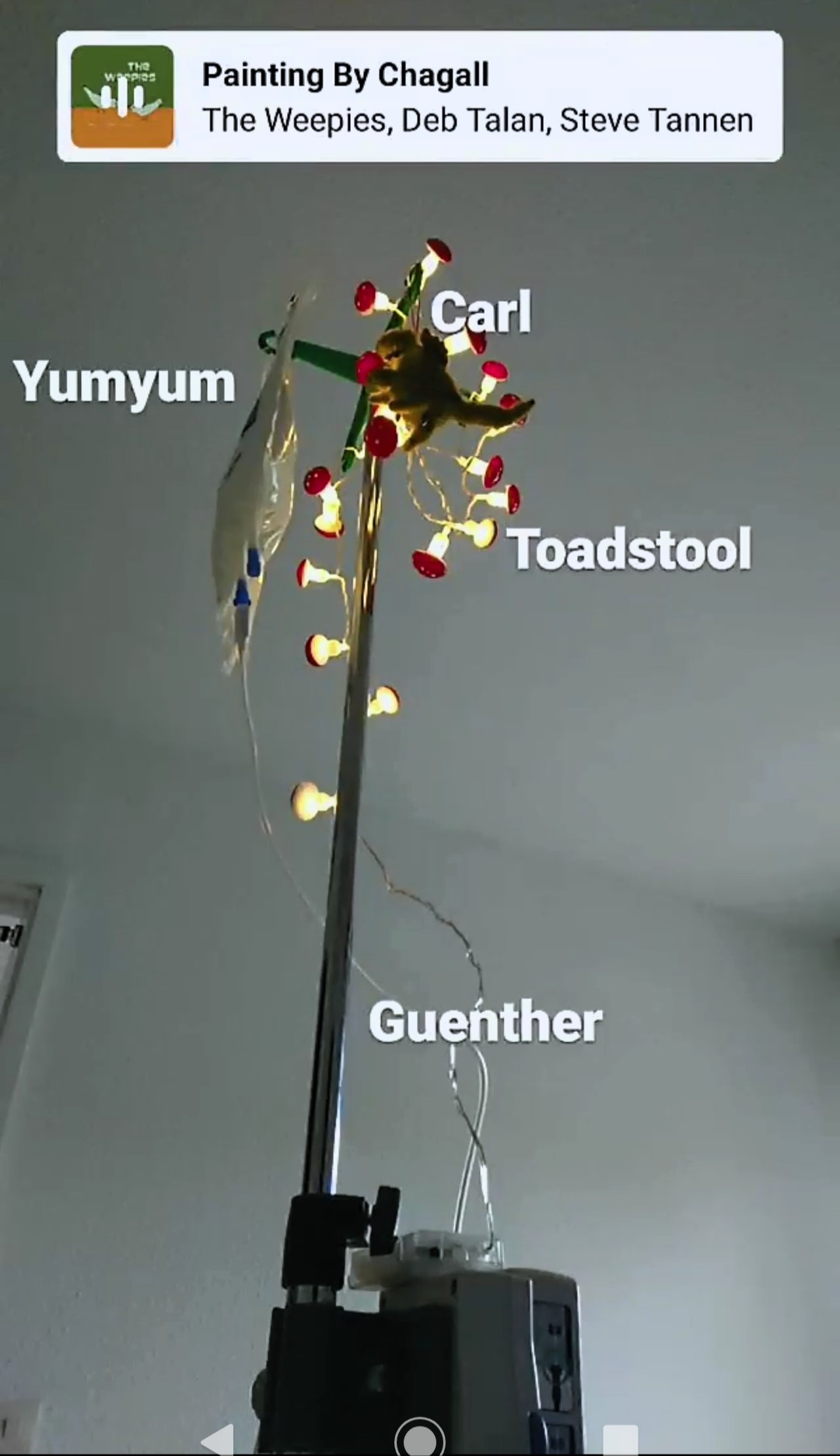 If symptoms persist, sufficient nutritional intake might be only possible via TPN (total parenteral nutrition) which is given iv (intravenous) and bypasses the gut. Basically, the fluid is already broken down into glucose, proteins, lipids, minerals trace elements, vitamins and electrolytes***** and can be further added with additional vitamin or mineral injections if needed. For a short time it can be given peripherally (i.e. over a simple venous access), but afterwards a central venous catheter (max 2 weeks), a port, hickman line xx or picc line are necessary. Depending on your conditions and balancing the risks and benefits the doctors will decide which is the best option. They are all inserted in such a way that they end in a major vein from the heart. Many Cipo patients indeed totally depend on TPN since the intestines have completely failed. It should be the last (or penultimate) option as it is often accompanied with infections leading to sepsis, damage of other organs e.g. the liver and it is not always possible to feed iv life-long. If there is no other option people are let to starve. Endoscopic decompression with the help of tubes to the stomach, duodenum, colon and rectum might bring relief as well. Tubes help to reduce intestinal dilation and a good alternative for a surgery. This is often done in the acute case or in case of a volvulus which can occur in Cipo patients. In severe forms patients are being fed iv and have to drain their stomach and/or colon every few hours, because the body is unable to move own digestive content (also without oral feed).
If symptoms persist, sufficient nutritional intake might be only possible via TPN (total parenteral nutrition) which is given iv (intravenous) and bypasses the gut. Basically, the fluid is already broken down into glucose, proteins, lipids, minerals trace elements, vitamins and electrolytes***** and can be further added with additional vitamin or mineral injections if needed. For a short time it can be given peripherally (i.e. over a simple venous access), but afterwards a central venous catheter (max 2 weeks), a port, hickman line xx or picc line are necessary. Depending on your conditions and balancing the risks and benefits the doctors will decide which is the best option. They are all inserted in such a way that they end in a major vein from the heart. Many Cipo patients indeed totally depend on TPN since the intestines have completely failed. It should be the last (or penultimate) option as it is often accompanied with infections leading to sepsis, damage of other organs e.g. the liver and it is not always possible to feed iv life-long. If there is no other option people are let to starve. Endoscopic decompression with the help of tubes to the stomach, duodenum, colon and rectum might bring relief as well. Tubes help to reduce intestinal dilation and a good alternative for a surgery. This is often done in the acute case or in case of a volvulus which can occur in Cipo patients. In severe forms patients are being fed iv and have to drain their stomach and/or colon every few hours, because the body is unable to move own digestive content (also without oral feed).- If colonic inertia is the main problem, patients may benefit of an artificial bowel outlet via stoma (bowel emptying into a bag basically which can be temporary or long-term), along with removal of the larger colon or parts of it (especially if this is the major affected organ and simply redundant). The end can be attached to the remaining part of the colon (colostomy) or smaller bowel (ileostomy) with a colectomy i.e. removal of the large intestine. If only the colon is affected there is the possibility of a total colectomy or a subtotal colectomy where you remove the whole larger bowel or the affected part of it. If the rectum is not affected it can be attached back to the smaller bowel or left part of the larger bowel, respectively (with ileorectal anastomosis). Prior to a colectomy one should be sure that the patient benefits from it since there have been many cases where the colon was removed, but the dysmotility in the small intestine made a symptom relief impossible or progressed over time. Often constipation may improve, but patients still suffer from pain and bloating which might then be caused by underlying co-existing IBS.
- In the past years sacral nerve stimulation by pacemakers, for stomach and bowel, have been tried out in certain patient groups, but haven’t shown much success. In patients with fecal incontinence and urinary problems it does show better success rates. It isn’t such an invasive surgery and might work for some patients suffering from gastroparesis and lower bowel dysmotility e.g. from spinal cord injury or pelvic floor dysfunction. It increases vagal activity by electrical stimulation of sacral nerves. Prior to the final insertion the doctors can test its effect and the impulses can be changed by the doctor and patient until successful or optimised. The pacemaker has to be renewed every few years in another minimal invasive surgery.
- When all options have been tried out and TPN isn’t possible anymore due to liver failure, loss of venous access or accumulation of infections doctors might suggest an organ transplant of the smaller bowel and colectomy. This surgery is very complicated and risky with a high mortality and low success rate as well as complications post op such as rejection and dumping syndrome. If successful, patients are often able to tolerate oral feeds again and is a life-saving surgery. If the stomach and other organs are also involved things become even more complicated, multi-organ transplants rarely go well.
- Any alternative ways such as meditation, TCM, cognitive therapy etc should be considered as additional support. Psychological support (simply because of the daily struggles), but also to strengthen gut-brain connection and manage the relation to food is necessary. Patients that are able to eat, often develop an ill relation to food as it causes negative effects or restrict their eating to food that causes less problems, fasten when symptoms are too severe etc. This can result in either a false diagnosis of an eating disorder and lack of medical treatment or indeed a resulting eating disorder from this medical underlying condition. If latter is treated one should make sure that patients don’t remain in this psychological pattern or are literally afraid of eating. Cognitive behavioural therapy (talk therapy and similar that help patients to become aware of how negative thinking affects symptoms), relaxation therapies, multicomponent psychological therapy (different measures from above), hypnotherapy, mindfulness meditation training, … should be tried out. Being afraid of eating can become its own condition. One should prevent AFRID (Avoidant Restrictive Food Intake Disorder) where patients limit the amount as well as types of food due to the symptoms they cause/think they cause – unlike anorexia, but it can develop into a proper eating disorder. Also, both lead to malnutrition and decrease of calorie intake. It often occurs with MALS and SMAS as well, because the compressions cause postprandial pain, vomiting and nausea. Further, resulting cibophobia (fear of food) and emetophobia (fear of vomiting resulting from the negative and life-limiting experience of vomiting due to the dysmotility) should be prevented or tackled. I can speak from my own experience that I haven’t touched anything with onion or garlic in the past years, even in phases with no gastro symptoms whatsoever, as I am simply afraid of the massive pain from the distended bowel. Last summer it took me a whole morning of meditation to eat a small bite of a hard-cooked egg as it reminded me of the very terrible time after the first surgery where it caused the severest cramping I have ever had. Lastly, patients that don’t tolerate anything by mouth should have psychological support. Eating is a natural need of human beings and so much more than only an energy provider.
- Hypoganglionosis: Decreased number of nerve cells in the ENS of the intestinal wall (especially in the myenteric plexus) which clinically manifests as motility disorders such as Gastroparesis (stomach), slow transit constipation (colon), CIPO/enteric dysmotility (small intestine), achalasia (esophagus)
- Aganglionosis: Complete lack or loss of nerve cells (most famous form is the aganglionosis only inside the rectum = Morbus Hirschsprung)
- Dysganglionosis: pathological changes in the ENS e.g. immature ganglia cells (sometimes it is also an umbrella term for hypoganglionosis, intestinal neuronal dysplasia,…)
- (myenteric) ganglionitis: inflammation of the ganglions
- In an ileostomy an opening (‘stoma’) from the small intestine through the abdominal wall is created. The products that are normally transported further to the large intestine are collected in a bag. It can be temporary (i.e. removable, also called loop ileostomy) e.g. after surgeries for the affected intestine to give it time to heal i.e. the rest of the intestine is still kept and a permanent ileostomy e.g. after the removal of parts of the intestine (the large intestine is often removed in colonic inertia, certain cancer types or chronic inflammatory bowel diseases). In severe dysmotility those ileostomies can be used for venting.
- A colostomy is the same, but in the large intestine which can also be permanent or temporary. For dysmotility, there is also a caecostomy tube which makes irrigation possible, when the colon is affected and enemas aren’t possible anymore.
- A PEJ (percutaneous endoscopic jejunostomy) is a tube that leads into the jejunum (small intestine) through the abdominal wall. It can be used for feeding, where it bypasses the stomach and part of the small intestine, and application of meds. In dysmotility it can be used for decompression, but the risk of dislodgement is high. It can either be placed in a lap surgery, x-ray guided or during endoscopy. After a month it can be swapped with a J Button for long-term usage. This one sits flat on the surface skin and you can then connect different extensions to it. For small intestine dysmotility one can use it for feeds, meds and irrigation in and venting out.
The acute pseudo-obstruction often needs immediate surgery, although one should first try conservative treatment first e.g. with the help of parasympathetic drugs (if a mechanical cause was excluded).
Prognosis? Unsatisfactory. There are not many specialists or clinics specialising in the diagnosis and treatment of motility disorders, most options are in the US and the UK . For Cipo there is no cure.


Tests in Detail
- H2 breath test
- Lactulose to test for the transit duration between oral intake up to the large intestine
- Glucose to test for SIBO (make sure that they also measure your glucose levels at the same time)
- C13 breath test
- acetate/octane acid to test for stomach emptying of solids and fluids
- Urea to test for stomach infections (helicobacter pylori)
- Triglyceride to test for pancreas function
for motility. Combined testings can show how fast your small intestine transports the fluid or solid samples.
- H2 breath test
- Lactose
- Fructose
- Sorbitol
- Sucrose
to check for carbohydrate intolerances, respectively. Follow the instructions of your doctor. It is very important to stay nil by mouth, don’t brush your teeths or chew gum etc as they can manipulate the findings. A high fasting value can point towards intestinal problems as well. Those tests trigger symptoms like bloating, pain, nausea, diarrhea – so be prepared and let them know what your symptoms are. The doctors can then analyse the results according to the symptoms. Also, I would recommend bringing some distraction with you since you are not allowed to move much and in case of motility testing the duration can be very long (if you suffer from dysmotility, too). Those breath tests aren’t always that accurate, false positive and negative tests are not that rare. Hence, I would recommend to only evaluate them along with other motility and intolerance testings e.g. a scintigraphy and biopsies.

- The hinton test is a transit test that can distinguish between different dysmotilities in the colon. Over six days you take one pill every day at the same time, on day seven an x-ray is taken (sometimes also after 3 and 7 days) at that time. Your doctor can then evaluate how far the pills (that break into many small different parts) got. Normally, ¾ of the markers should be evacuated via stool, a normal transit lasts between 60 and 90 hours. If there are still markers left you are doctor will be able to see whether there are certain segments that are slowed down, whether the whole colon is slow (evenly distributed markers in the colon – the slower the motility the further apart from the rectum) or whether you suffer from an outlet obstruction when the marker collect in the rectum. Mechanical obstruction or dys/atony in certain segments, slow transit constipation up to colonic inertia and outlet obstruction (Morbus Hirschsprung, pelvic floor dysfunction), respectively. One can also differ between functional constipation in IBS-C where the whole transit time is normal, but patients suffer from (subjective) constipation and functional constipation where the transit duration is indeed slowed down – both can have very similar symptoms. During the intake of the pills you are not allowed to take any meds that affect the motility. Make sure that the x-rays are always taken in the same position i.e. standing or laying.

- phase I: minor or no contractile activity
- phase II: intermittent and irregular contractions
- phase III: maximal contractions of slow waves
that repeat every 90min (that’s why the manometry takes so long before food intake, some guidelines want to see at least one cycle in 4 hours). The patterns should be forwarded from the antrum to the jejunum. After food intake the waves should be amplified in all segments, more frequently and take at least 2 hours depending on the meal’s nutritional content. Finally, the activity is replaced by new MMCs.
According to the amplitude of those waves and their pattern the motility can be analysed with all its details. Depending on those results it will be easier to suggest an effective treatment. For example, patients that suffer from a generalised intestinal dysmotility don’t necessarily benefit from a colectomy to treat intractable constipation whereas patients that ‘only’ suffer from colonic atony do. Manometry findings should be evaluated along with the other motility testings, symptoms and conditions of the patients. Based on abnormal findings of the manometry alone not much can be concluded. If the contractions follow a normal pattern, but the amplitudes are too low (<15mmHg) it points towards a myopathy. If the amplitudes are sufficiently high, but the patterns are abnormal and uncoordinated, it indicates neuropathy. Both can exist at the same time. Hypomotility after food intake is often seen in dysbalances of the ANS. Burts of waves can be seen in neuropathic intestinal pseudo-obstructions. For further information you can have a look at the publications online.
Make sure to follow the doctor’s rules regarding fasting and certain meds you should stop (motility increasing and decreasing ones). The examination takes many hours, I recommend bringing something for distraction.

- The full-thickness biopsy/resection can give additional information. Here, a full part of the intestinal wall up to the serosa is resected and analysed (normal biopsies only take the (sub)mucosa). A full thickness resection of the colon can be done via colonoscopy today (with the FTRD system that is also being used to resect polyps, directly with the resection the colon wall gets closed with a metal clip and complications like inner bleeding or infections are reduced; prior you will also get antibiotics), for the small intestine the probe is resected in a laparoscopic surgery. The preparation is the same as for a colonoscopy (your intestines must be clean to not risk an infection, as clearing my bowel obviously doesn’t work, they flushed it prior) and the device is simply mounted on the colonoscopy probe, you will be sedated and afterwards observed for internal bleeding. Make sure that your doctor knows how to take those resections, prepare them and send them to pathology (they have to be cooled in a certain way etc). Inner bleeding or infections are rare, but you should be monitored and blood transfusions should be available in case. The biopsy can show abnormalities such as:
- Aganglionosis (Morbus Hirschsprung) meaning complete loss of nerve cells
- Hypoganglionosis meaning decrease of nerve cells of the Myenteric Plexus
- Increase in giant ganglia or other nerval changes suggesting intestinal neuronal dysplasia
- Changes in the muscular layers pointing towards visceral myopathy
- Inflammations e.g. IBDs as causes for dysmotility, inflammatory lesions of the Muscularis Propria are common in Crohn’s
- Changes in the connective tissue e.g. absence of the tendinous plexus layer suggesting intestinal desmosis
- Virus ganglionitis, rare cases where virus infections can disturb peristalsis (e.g. Chagas, EBV, Varicella Zoster)
- It can also provide information whether the condition is acquired or congenital.

(…) to be continued.
Resources
- ANMS in the US
- BSG and the neurogastro group at QMUL in the UK
- visual explanations
- Neurogastro journal
- Nature articles
- pathology: Prof Meier- Ruge and Dr Bruder
- videos of
- podcasts of the neurogastro journal, Dysautonomia support network, ‘Gesunder Darm’
- Leitlinien der DGNM

*Stay tuned for more:
- Gastrointestinal dysmotility in dysautonomia
- Achalasia
- GERD
- Dysphagia
- Gastroparesis
- Dumping Syndrome
- Functional Dyspepsia
- Cyclic Vomiting Syndrome
- (Severe forms of) IBS
- Short bowel syndrome
- Colonic inertia, slow transit constipation
- Pelvic floor dysfunction
- Hirschsprung
- …
** In fact, it was first diagnosed in 1948 where a tumor invaded the celiac plexus which is, as described affects the ANS.
***micronutrients are nutritions that your body can’t build on its own and we need to survive. They don’t give energy, but they make the absorption and resorption of the energy giving carbs, fats and proteins possible.
****prokinetics, allowed in Germany:
- Erythromycin which increases the quantity and intensity of gastric contractions (some evidence also for the smaller bowel), similarly Domperidone (only iv and max 7 days), mainly for gastroparesis.
- Metoclopramid (MCP) which is also against nausea by increasing the motility in the stomach and bowel. It is a D2-Antagonist und 5-HT4-Agonist meaning it decreases the dopamine receptors and increases the serotonin receptors, respectively. It shouldn’t be a medication one takes very often.
- Prucalorpids (Germany: Resolor) increase bowel motility as 5-HT4-Agonists, mainly for slow transit constipation, colonic dysmotility where all other laxatives have failed.
- In the UK and US, Cisapride for gastroparesis and Motegrity for stomach and bowel dysmotility are often used.
- All can have quite severe side effects.
*****It is very important that the nutritional intake is somehow managed and patients are not sent home to starve. This is not only life-limiting, then life-threatening, decreases their QoL and causes further health problems that need to be tackled, but also often directly worsen symptoms. Additionally, refeeding syndrome can be a huge problem if patients decrease calorie intake for a long period and don’t have further support. When starting nutritional support, specialists have to install a safe and efficient plan. Refeeding syndrome can even lead to organ failure and even death due to metabolic dysbalances when introducing the feed (electrolytes, vitamin levels, fluid etc can play crazy). One has to constantly check the blood levels and general state of the patient and react if levels are off. Malnourished victims in countries that suffer from war and hunger also suffer from this condition when adequate food intake is possible. Symptoms range from severe tachycardia, epilepsy, coma to death. One should start with a low and slow introduction of feeding and the right substitution of electrolyte and vitamins from there on.
Dietary Advice
******High calorie drinks – an overview
Resource
- Protein: high protein – 30% milk protein, 45% carbs (glucose syrup, sucrose), 25% fats (rapeseed oil), no fibre, 1.25kcal/ml (Vanilla suitable for low fodmap)
- 2.0: moderate protein, high calorie density (volume sensitive) – 17% milk protein, 44% carbs (glucose syrup, sucrose), 39% fats (rapeseed oil), no fibre, 2kcal/ml (Vanilla suitable for low fodmap), for oral and tube feed use
- 2.0+Fibre: moderate protein, energy dense, added fibre – 18% milk protein, 40.5% carbs (glucose syrup, sucrose, oligofructose), 39% fats (rapeseed oil), FOS/GOS fibre, 2kcal/ml (Vanilla suitable for low fodmap), for irregular bowel movements
- Plus: moderate protein and high energy – 15% protein (Sodium Caseinate, Calcium Caseinate and Soy Protein Isolate), 58% carbs (Maltodextrin, sucrose), 27% fats (sunflower, rapeseed oil), no fibre, 1.5kcal/ml (Vanilla suitable for low fodmap), for oral and tube feed use
Fresubin
- Original Drink: moderate energy- 3.8% milk protein, 13.8% carbs (Maltodextrin, sucrose), 3.5% fats (sunflower, rapeseed oil), without fibre, extra vitamin D, 1kcal/ml
- 3.2kcal Drink: high condensed energy, only 125ml to drink, high protein – 16% milk protein, 28% carbs (Maltodextrin, sucrose), 16% fats (sunflower, rapeseed oil), little fibre, extra vitamin D, 3.2kcal/ml
- 5kcal Shot: high energy, low volume, high fat, 4% carbs (sucrose), 54% fats (MCT, rapeseed oil), little fibre, extra vitamin D, 3.2kcal/ml
- 2kcal Drink: high energy and protein – 10% milk protein, 22% carbs (glucose syrup, Maltodextrin, sucrose), 8% fats (sunflower, rapeseed oil), with and without fibre, extra vitamin D, 2kcal/ml, sweet and savoury options
- Protein Energy: high energy – 6% milk protein, 19% carbs (Maltodextrin, sucrose), 6% fats (sunflower, rapeseed oil), with and without fibre, extra vitamin D, 1.5kcal/ml
- Provide Xtra: for malabsorption, digestion disorders, CEDs – 33% carbs (Maltodextrin, sucrose), 4% pea protein, without fibre, extra vitamin D, 1.5kcal/ml, juice-like, milk-free
- Powders you can add in water or milk: fibre, protein, Calshake (energy and protein rich),
- For certain illnesses such as diabetes (Diben), renal and liver diseases (Renal, Hepa), swallowing disorders (Thickened) etc
Forti
- Similar to above (but less sugar in the carb section, less artificial ingredients in my opinion) with
- Fortimel Compact + fibre, + protein (also Extra with even more protein), + energy, 1.5 or 2.4kcal/ml (less volume)
- + multifibre (soluble and insoluble), Jucy (no fats, no milk)
- For certain conditions (wound healing disorders: Cubitan, diabetes: Diasip, cancer: Care, CEDs and other gastro conditions: Elemetal028 – no milk or fibre, only MCT fats)
- For muscle improvement (Fit Pulver, Ft Energy Plus),
Ensure (as above, not as dense)
- Original
- Plus: energy dense
- High Protein: 16g, added minerals and vitamins
- Max Protein: 30g, 1g sugar only
- Plant based protein: bean and pea
- Clear: fat and milk free
- Compact: high density
- Surgery: post op for immune improvement, Pre-surgery: carbs to prepare for surgery
- Enlive All-in-one: protein and ‘complete balanced nutrition’
Most are available in different flavours (mostly vanilla, strawberry, cappuccino, strawberry, chocolate, neutral, wild berries for the milk ones and fruit flavours e.g. orange, apple, cassis for the non-milk based ones). The coffee flavoured ones sometimes contain caffeine. In my opinion, they are all very sweet and partly very disgusting, so if drinking is possible I would dilute them or mix them (e.g. some of the cappuccino flavour into your coffee etc). There doesn’t seem to be many savoury options (e.g. Resource Soups).
Low fodmap focussed high calorie drinks from Nestlé are available in the US and Australia (ProNourish). It seems that in the UK one favours Ensure, in Germany Fresubin, Boost (based on Glucose Syrup, Canola Oil, Acid Casein (From Milk), Soy Protein Isolat mainly) in the US (also, I am not evaluating those drinks here and certainly not advertising them – in my opinion, they re definitely not healthy and there are some companies that seem to rule the market and make quite a lot of money with it; on the other hand they can help to keep the weight stable or even prevent malnutrition). Recall that they don’t contain micro nutrients*** and you can do a lot with them. Human’s milk has the lowest part of proteins and humans don’t need much protein (if you are an athlete this doesn’t apply), in the sense that it should be carbs-fats-proteins. Nevertheless, many people consume proteins in large portions as they think it is healthy, there are many weight losing myths about increasing protein intake etc – this is unhealthy! In fact, it can cause major problems, from a dysbalance of the bowel flora and constipation to kidney and liver damage. Same with low carbs and other diets, it is unhealthy as soon as one shifts away from a balanced diet. Only if you have conditions that need special diets (which your doctors will explain to you) or specifically need high levels of proteins after surgeries or similar, one should change the food content. Most of the drinks have their parts from one or two sources, but diversity is always better e.g. getting proteins from plant and animal sources, from milk products and veggies etc.
I have seen new drink meals, vegan and free-from stuff (it seems to attract people – note: free-from doesn’t mean it is healthier!) such as Huel, Mana and This is food which differ from the above listed ones as they don’t target malnourishment (probably rather the opposite as the increased protein part should increase satiety), but rather increased protein intake (Mana has 40% protein, for example) which I don’t recommend unless you are doing sports/for muscle growths. They are also not proper meal replacements as they don’t give the right balance of nutrition. I actually tried Unmilk at some point which is based on oat milk with additional vitamin D and B12, 20g oat and pea protein, fiber which doesn’t fulfill the criteria, but tasted quite ok. Betrand seems to be the only drink that is based on organic ingredients and doesn’t contain any artificial stuff.
Balanced supplements can be bought over the counter, such as Complan or Meritene. Protein (Prosource (Plant), Clinutren, Protifar) or energy (Calogen, Nutricia – fat emulsion) only supplements or similar can be added as well, such as Optifibre (fibre for bowel regulation) etc.
They are not all easy to digest and can cause early satiety, nausea or exactly the same symptoms when you take solid food (if you suffer from gastro problems).
Most are free from lactose (not milk) and gluten, but talk with your doctors if you have any intolerances. Drink it cooled, slowly and within 24h (shots can stay in the fridge two weeks after opening). If possible, one can also use the drinks to enrich your food (I would recommend the neutral taste or powder) e.g. in the yogurt, soups etc.
If you suffer from malnourishment, severe underweight due to illness you can get them prescribed by your GP – otherwise those drinks are really expensive.
Recipe collection and some advice
….which suit low fodmap needs, easy to digest, for low motility etc.
Every patient is individual. Some safe foods for one patient can cause a major flare in another, so obviously adapt cooking to your body. I think the best way is to try out, take flares into account and listen to your body and intuition. Below I will add more recipes every few weeks.
Recommendation 1: Broth powder without artificial ingredients, onions/garlic, yeast, sugar – low fodmap, liquid diet, nutrients and vitamins (takes some time)
- Peel and cut veggies into small pieces (safe ones, may need adaption: zucchini, carrots, parsley root, tomato, fennel, spinach or mangold, pumpkin – you can also use leftovers or make two different ones, too many different ingredients may upset the gut)
- Add safe fresh herbs and spices (parsley, basil, sage, mint, ginger, turmeric, coriander, cumin, some salt – for POTS sufferers a bit more and it should be at least an eighth of the veggie weight, pepper – only if tolerated, lemon grass… grounded or powdered)
- Chop in a mixer
- Spread onto a baking tray and put into the oven (preheated at 80 degrees Celsius)
- Leave it in the oven for 4 hours and open the door a few times such that the fluids inside the veggies can leave the oven (you can also keep the door a little bit open), keep the mass evenly mixed and heated
- You can now add dried herbs (rosemary, fennel seeds, thyme, fenugreek…) and mix it again (if you have a fine grating mixer, make it to pulver)
- if properly dried fill in a jar that can be hermetically closed
It should be used within four months and as usual one or two tsps in a cup with hot water.You can also use it to enrich other soups or fish/bone broths.
Recommendation 2: By now there are also products with the label low fodmap (e.g. by Schaer, Monash – they also have a app with lists, recipes and a dietary log) which you can trust. Schaer also provides gluten-free products, but gluten-free isn’t included in low fodmap i.e. if you don’t suffer from a gluten intolerance you can eat gluten. In fact, wheat bran, for example, is a good source of fiber, plant-based proteins and minerals (for IBS). In the UK and US there are special (online) shops for low fodmap products only. Whole Foods and Walmart have a good diversity here. The common Bioläden in Germany do so, too. Have a look at products of Frusano, for example. Schaer biscuits or pretzels, Trek protein bars, a rice cake, salted popcorn, seaweed snacks… there are some snacks one might still enjoy on a low fodmap diet. As usual, self-made is always the best or simply safe portions of some fruit or nuts. Alternatives for milk and soy products are available on mass, swap your wheat products with some sourdough or spelt product and so on. Again low fodmap doesn’t mean gluten free and there are also many gluten free products that are high in fodmaps (e.g. soy or bean flour), be careful! There is a lot of information on the internet.
Recommendation 3: Balanced is always the best. Unless your doctors and nutritional experts recommend a no-diet you should try to include foods from all categories e.g. on a low-fat diet you should still add some fats, possibly the ones that are easy to digest and the ones you tolerate well.
Recommendation 4: And chew, chew, chew. Ignore the people that look weird at you when you eat a few bites in an hour only. Have your own pace. Chewing is always good.
Recommendation 5: Look out for high fodmaps that love hiding in processed foods (which one should ideally eliminate) such as wheat starch, honey, corn sirup, sweeteners that end with ol (sugar alcohols in many sugar-free gums and candies or drinks), agave, FOS, HFCS and isomalt. Be careful for any onion or garlic powder, chicory root, …
Recommendation 6: Add extra calories with a spoon of linseed/hemp oil in yogurt, soups etc; high calorie powder (e.g. if tolerated calshake) in literally everything that is liquid; if tolerable cream (also possible on soy/almond basis etc) – healthy fats help the most in gaining weight. For additional protein (e.g. after surgeries) add protein powder such as pea or hemp powder. Try to limit low calorie but high volume-food and especially limit low-nutrient foods. Find alternatives e.g. if nuts and seeds have to be eliminated make your own nut or seed butter.
Sunflower seed butter, low fodmap, high calorie, high energy, nut free
- Preheat the oven to 200 degrees celsius and spread Two cups of hulled sunflower seeds on a baking tray
- Roast for 15min and keep mixing them every few minutes
- Cool and mix in a food processor – be patient, it will get soft
- When lumps are forming, stop and add some linseed oil and a pinch of salt
- Mix again until creamy
- Fill in a jar that can be hermetically closed
- Alternatives: hemp seeds, pumpkin seeds, sesame
Nut butter, low fodmap, high calorie, high energy
- As with the sunflower seed butter, but use macadamia nuts, peanuts or tiger nuts
- Be careful when roasting as they might burn earlier
On a low fodmap diet don’t eat the whole jar in one go lol.
Recipes, stay tuned for more



