This post is mainly about neurogastro stuff and some recommendations in the end, if you want to read about absurdism, stones, optimism, Urvertrauen and donuts stay tuned for the next post. I added more on dysmotility and parenteral nutrition.
Can You Trust Your Gut?
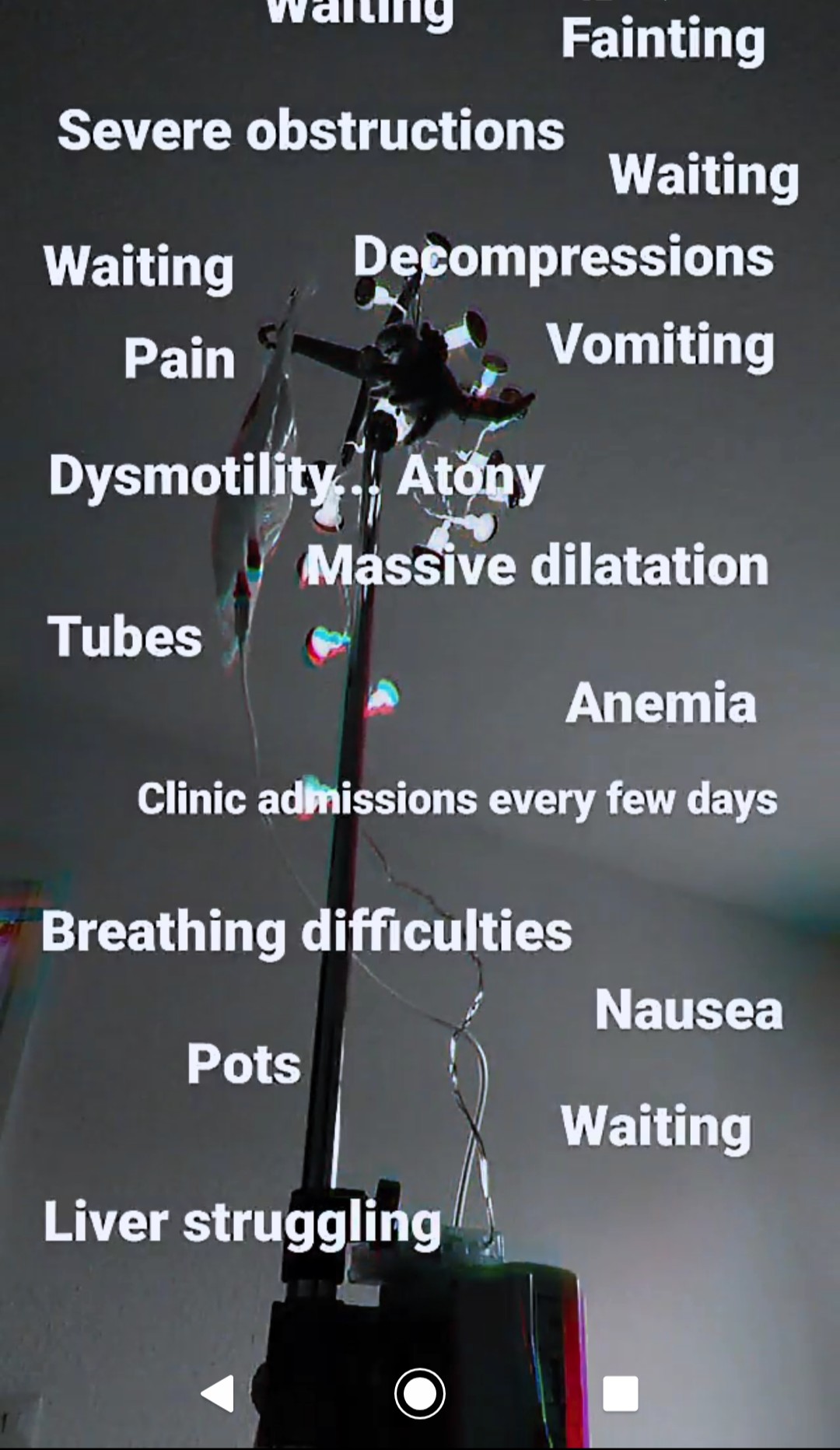
The situation hasn’t changed much other than the subileus symptoms have been increasing, my abdomen is dilating more and more and my liver is struggling. I am definitely not doing well. I am sick of clinic stays, doctor visits, A & E visits, those long drives to specialists, tests and interventions, calls and emails, I am sick of being sick. I had all important neurogastroenterology tests and interventions that confirmed the issues. Hopefully, the results will guide us towards some kind of therapy. The small intestine manometry and full thickness resection (see below for detailed explanations) should provide us with important answers.
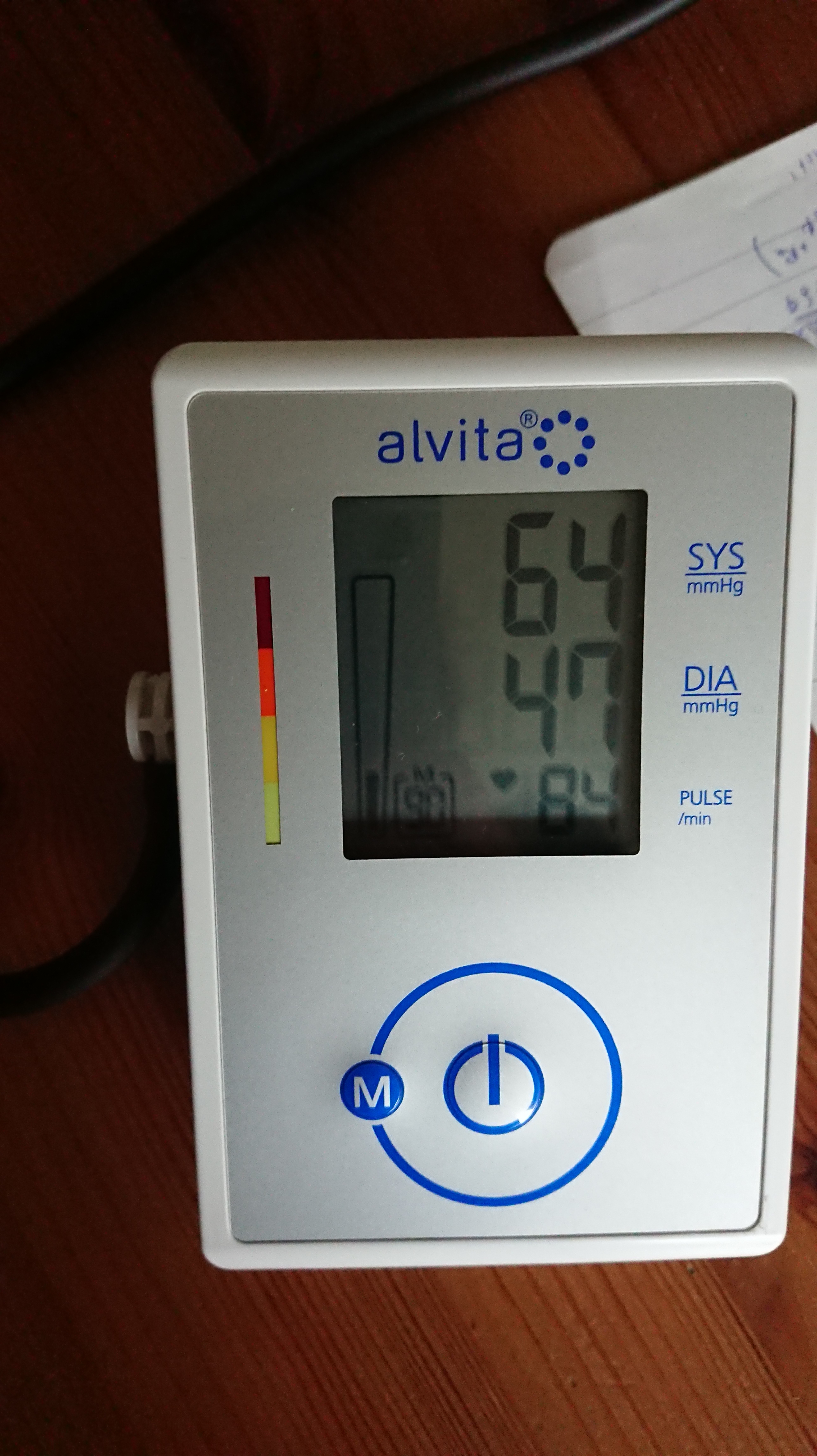
 My weight has stabilised around 40kg+/- again, preparing parenteral nutrition every day and being hooked up to Guenther or Franklin has become a new normal. I try managing the pain from dilatation, nausea, weakness, quite severe dysautonomia, clinic stays and doctor visits and seemingly endless waiting with my usual techniques some of which I will explore in the next two posts. I wonder when I am going to explode, I hope it will be a nice colourful firework. The dilatation is so severe that it compresses my diaphragm and makes it difficult to breathe. I don’t give up. Despite all, I convince my mum to go outside with me when I am not in the clinics, to walk a few more metres, to laugh about our situation, to stay hopeful. When in the next moment I act ok until I have to be honest that I am going to faint any minute. My blood pressure drops, I get pale like Kniepsand and sink to the ground; my mum’s blood pressure rises, fear. And the cycle continues.
My weight has stabilised around 40kg+/- again, preparing parenteral nutrition every day and being hooked up to Guenther or Franklin has become a new normal. I try managing the pain from dilatation, nausea, weakness, quite severe dysautonomia, clinic stays and doctor visits and seemingly endless waiting with my usual techniques some of which I will explore in the next two posts. I wonder when I am going to explode, I hope it will be a nice colourful firework. The dilatation is so severe that it compresses my diaphragm and makes it difficult to breathe. I don’t give up. Despite all, I convince my mum to go outside with me when I am not in the clinics, to walk a few more metres, to laugh about our situation, to stay hopeful. When in the next moment I act ok until I have to be honest that I am going to faint any minute. My blood pressure drops, I get pale like Kniepsand and sink to the ground; my mum’s blood pressure rises, fear. And the cycle continues.

In April, I had some breath tests to confirm the issues again. There are
- H2 breath test
- Lactulose to test for the transit duration between oral intake up to the large intestine
- Glucose to test for SIBO (make sure that they also measure your glucose levels at the same time)
- C13 breath test
- acetate/octane acid to test for stomach emptying of solids and fluids
- Urea to test for stomach infections (helicobacter pylori)
- Triglyceride to test for pancreas function
for motility. Combined testings can show how fast your small intestine transports the fluid or solid samples.
And
- H2 breath test
- Lactose
- Fructose
- Sorbitol
- Sucrose
to check for carbohydrate intolerances, respectively. Follow the instructions of your doctor. It is very important to stay nil by mouth, don’t brush your teeths or chew gum etc as they can manipulate the findings. A high fasting value can point towards intestinal problems as well. Those tests trigger symptoms like bloating, pain, nausea, diarrhea – so be prepared and let them know what your symptoms are. The doctors can then analyse the results according to the symptoms. Also, I would recommend bringing some distraction with you since you are not allowed to move much and in case of motility testing the duration can be very long (if you suffer from dysmotility, too).
Those breath tests aren’t always that accurate, false positive and negative tests are not that rare. Hence, I would recommend to only evaluate them along with other motility and intolerance testings e.g. a scintigraphy and biopsies.
Further, another Hinton test
- The hinton test (sitzmark test) is a transit test that can distinguish between different dysmotilities in the colon. Over six days you take one pill every day at the same time, on day seven an x-ray is taken (sometimes also after 3 and 7 days) at that time. Your doctor can then evaluate how far the pills (that break into many small different parts) got. Normally, ¾ of the markers should be evacuated via stool, a normal transit lasts between 60 and 90 hours. If there are still markers left you are doctor will be able to see whether there are certain segments that are slowed down, whether the whole colon is slow (evenly distributed markers in the colon – the slower the motility the further apart from the rectum) or whether you suffer from an outlet obstruction when the marker collect in the rectum. Mechanical obstruction or dys/atony in certain segments, slow transit constipation up to colonic inertia and outlet obstruction (Morbus Hirschsprung, pelvic floor dysfunction), respectively. One can also differ between functional constipation in IBS-C where the whole transit time is normal, but patients suffer from (subjective) constipation and functional constipation where the transit duration is indeed slowed down – both can have very similar symptoms. During the intake of the pills you are not allowed to take any meds that affect the motility. Make sure that the x-rays are always taken in the same position i.e. standing or laying.
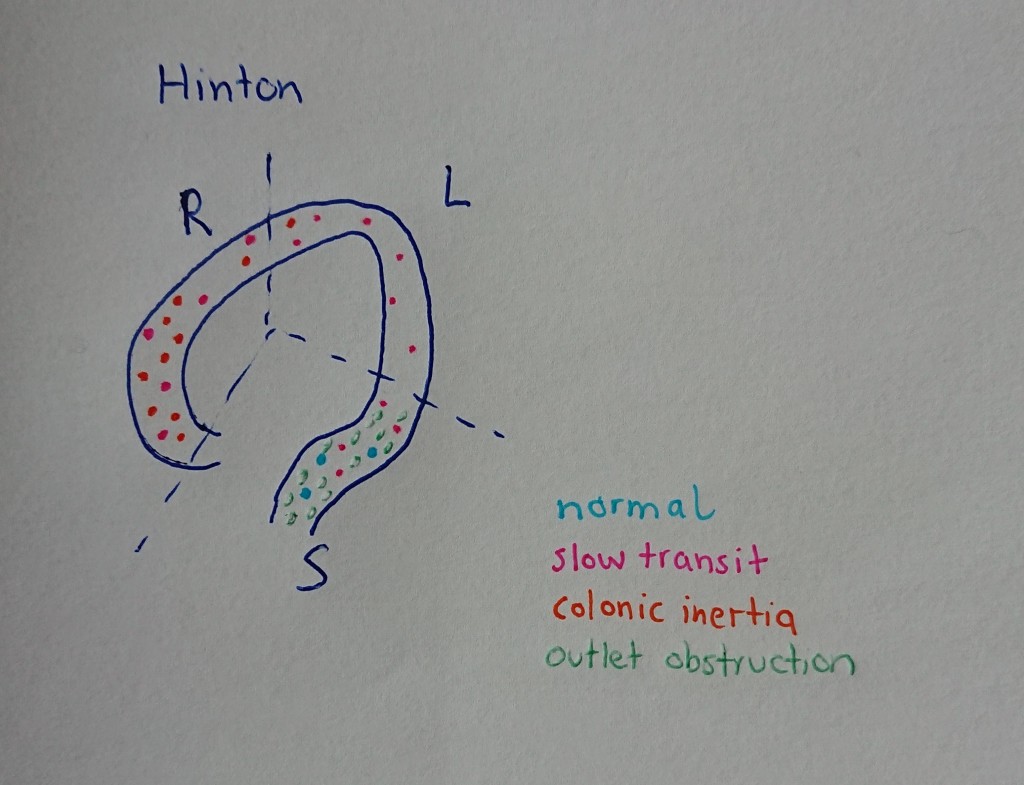
was conducted to see the extent of the colonic dysmotility/atony. A smart pill would have gotten stuck and having little plastic rings inside me is tolerable.
To look for the causes of constipation or evaluate whether a general intestinal dysmotility (from oesophagus to rectum) is present, we also did a
- An anorectal manometry measures the pressure and sensations in the rectum and evaluates whether the anal sphincter works. A balloon at a flexible catheter will be inflated inside the rectum. To evaluate whether the muscles are working properly you will be asked to squeeze and push as well as communicate when you feel certain sensations. Contractions and relaxations are measured. Prior to the test the rectum needs to be emptied. The test can evaluate causes of constipation and incontinence, it can also point towards Morbus Hirschsprung.
- An esophageal manometry measures the contractions, the coordination and force of the muscles in your esophagus. You will get a special tube through your nose into the esophagus and several pressure measurements are taken sober, whilst swallowing, swallowing of water, orange juice and some bites of rice. The test can provide answers for difficulties or pain whilst swallowing as well as regurgitation and unexplained chest pain. GERD (lower sphincter opens when it isn’t supposed to), achalasia (lower sphincter does not open when swallowing) or esophageal spasms (uncoordinated movements) can be diagnosed with the test. In scleroderma it is common that aside to the stomach or intestines the esophagus is affected and severe reflux and aperistalsis in the lower part is noticed. Both scleroderma and achalasia should be tested before further interventional treatment for GERD is planned. You won’t be sedated for those tests. I find lidocaine spray for NG tubes very comforting.
- A defecography also called an evacuation proctogram evaluates whether the actual process of defecation works. Barium paste will be injected into the rectum. You will then ‘go to the toilet’ and try having a bowel movement. The doctors will be able to follow your muscles’ reactions in a real-time moving MR imaging/ x-ray. You will also be asked to pinch and hold. Pelvic floor problems, fecal incontinence or functional obstructions due to pelvic floor dysfunction can be diagnosed with this test. Rectoceles (outpouching of the rectum), hernia and rectal prolapse (‘falled down’ rectum) are also visible. You will also need to have an enema prior the test.
My esophagus is not affected. Hence, if my intestines would allow it, I could swallow the yummy food. For me, my large intestine has been dilating more and more and the rectum is now so affected that I didn’t even feel the balloon. With the test you can diagnose a mega rectum. They are all not very pleasant tests, but very useful as they measure the functions directly and real time. To be honest I don’t want to think about how many doctors and nurses have seen me naked or how often I had tubes inserted from above and below for diagnostics or for treating (sub)ileus symptoms. It can be quite dehumiliating.
- A large intestine manometry: Here the contractions in the whole colon (some clinics only insert the tube up to the left flexure) are measured in the fasting state and after a high calorie meal which should stimulate propagating waves. You basically prepare for a colonoscopy and are awake during the test. A flexible tube that can measure pressure differences is inserted through the colonoscope. Make sure to stop any motility affecting meds prior to the test. Colonic inertia or slow transit constipation can be diagnosed with this test.
wasn’t necessary since my case is pretty clear and we would have needed another endoscopic decompression and emptying for it. Obviously, you want the intestines to have had as little manipulation as possible prior the testings.
In June, I had another stay in beautiful Bavaria. As described in the last post , a manometry measures the pressure differences. The small intestine manometry wasn’t very pleasant. Nonetheless, it was needed and I was very happy when I woke up with the tube inside me. Reason is that in the first attempts in April they didn’t manage to insert one as my small intestine kept pushing it back (due to the reverse peristalsis). If a small intestine manometry is scheduled they will insert the flexible tube (very similar to an NJ tube, so under x ray) via endoscopy under anesthesia (if you don’t wake up from it as I do) and after you have woken up, you will be connected to the manometry machine. Tubes in general aren’t very comfortable, but it could be worse. The manometry tube can take measurements at several locations in the intestine. The measurements start in the fasting state (at least 12h nil by mouth before as well, TPN had also to be stopped) for a few hours, then you get a meal and measurements continue after eating for a few hours more (it depends on the clinic, some will give you high calorie drinks, others a full meal – make sure to eat as much as possible in calories since the measurements will be more accurate then). The test’s duration varies from clinic to clinic, some also measure the intestinal pressure after the application of medication to see whether the intestine can actually be stimulated. Some measure whilst laying flat for the whole time, others are 24h measurements where you are also allowed to move and obviously sleep. The most difficult part for me was laying flat for so many hours, especially after food intake as it obviously triggers symptoms such as distention, pain, nausea, vomiting etc. Despite parenteral nutrition, many dysmotility patients are still able to eat, the food simply doesn’t get transported as it should (either it gets stuck or vomited out).

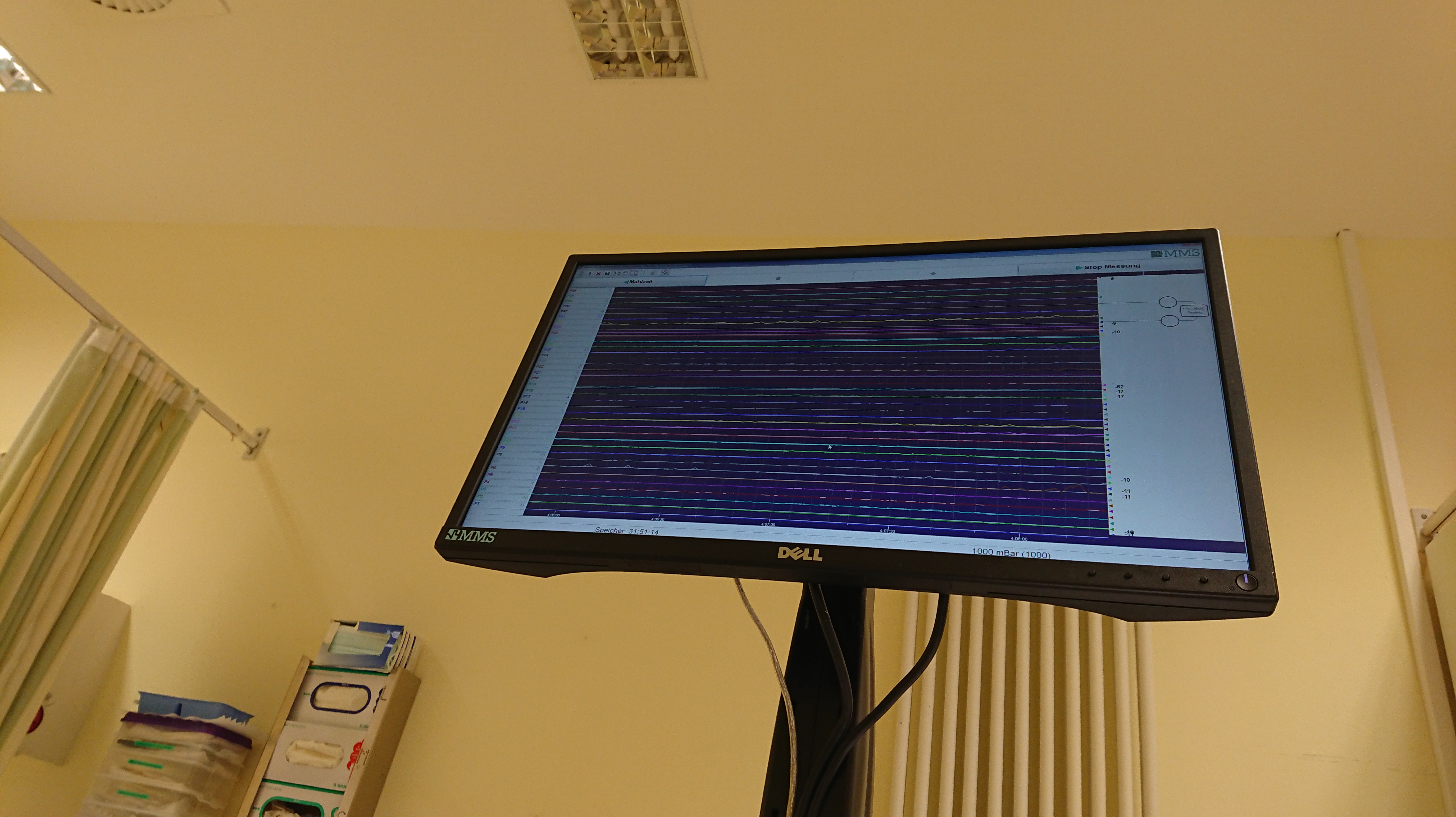
Normal motor activity follows very typical patterns and your doctor will be able to analyse the patterns afterwards. He can look for neuropathy (nerval problem)/myopathy (muscular problem) signs, signs for pseudo obstructions or enteric dysmotility. During the fasting state one should see cycles of MMC (migrating motor complex) which consists of
- phase I: minor or no contractile activity
- phase II: intermittent and irregular contractions
- phase III: maximal contractions of slow waves
that repeat every 90min (that’s why the manometry takes so long before food intake, some guidelines want to see at least one cycle in 4 hours). The patterns should be forwarded from the antrum to the jejunum. After food intake the waves should be amplified in all segments, more frequently and take at least 2 hours depending on the meal’s nutritional content. Finally, the activity is replaced by new MMCs.
According to the amplitude of those waves and their pattern the motility can be analysed with all its details. Depending on those results it will be easier to suggest an effective treatment. For example, patients that suffer from a generalised intestinal dysmotility don’t necessarily benefit from a colectomy to treat intractable constipation whereas patients that ‘only’ suffer from colonic atony do. Manometry findings should be evaluated along with the other motility testings, symptoms and conditions of the patients. Based on abnormal findings of the manometry alone not much can be concluded. If the contractions follow a normal pattern, but the amplitudes are too low (<15mmHg) it points towards a myopathy. If the amplitudes are sufficiently high, but the patterns are abnormal and uncoordinated, it indicates neuropathy. Both can exist at the same time. Hypomotility after food intake is often seen in dysbalances of the ANS. Burts of waves can be seen in neuropathic intestinal pseudo-obstructions. For further information you can have a look at the publications online.
Make sure to follow the doctor’s rules regarding fasting and certain meds you should stop (motility increasing and decreasing ones).
The examination takes many hours, I recommend bringing something for distraction e.g. a book, your phone to listen to music… (see below for my recommendations of songs and my latest book recommendation of Nature Cure).

The full-thickness biopsy/resection can give additional information. Here, a full part of the intestinal wall up to the serosa is resected and analysed (normal biopsies only take the (sub)mucosa). A full thickness resection of the colon can be done via colonoscopy today (with the FTRD system that is also being used to resect polyps, directly with the resection the colon wall gets closed with a metal clip and complications like inner bleeding or infections are reduced; prior you will also get antibiotics), for the small intestine the probe is resected in a laparoscopic surgery. The preparation is the same as for a colonoscopy (your intestines must be clean to not risk an infection, as clearing my bowel obviously doesn’t work, they flushed it prior) and the device is simply mounted on the colonoscopy probe, you will be sedated and afterwards observed for internal bleeding.
Have a look here, it is quite a smart concept. Make sure that your doctor knows how to take those resections, prepare them and send them to pathology (they have to be cooled in a certain way etc). Inner bleeding or infections are rare, but you should be monitored and blood transfusions should be available in case.
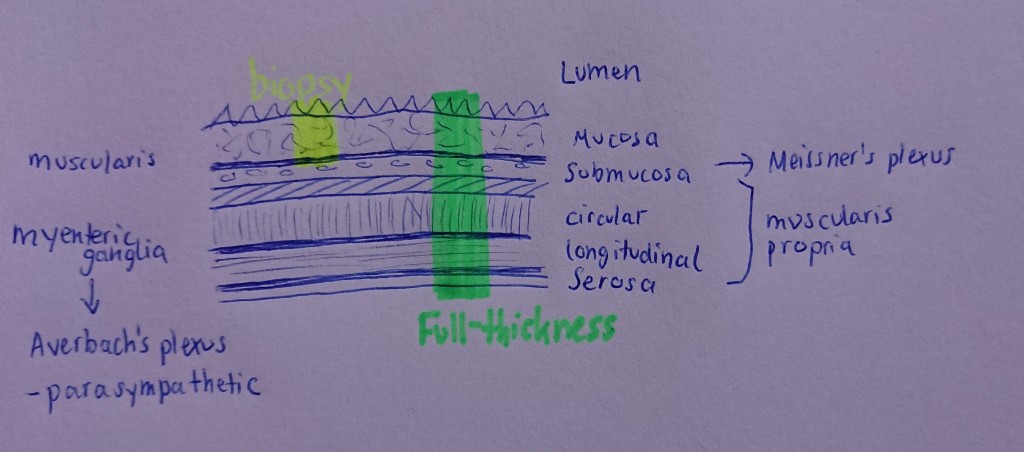
My biopsy is currently analysed in a neuropathology institute. If the problem is enteral (in contrast to the problem coming from the damaged ANS) the probe will show abnormalities, for example:
- Aganglionosis (Morbus Hirschsprung) meaning complete loss of nerve cells
- Hypoganglionosis meaning decrease of nerve cells of the Myenteric Plexus
- Increase in giant ganglia or other nerval changes suggesting intestinal neuronal dysplasia
- Changes in the muscular layers pointing towards visceral myopathy
- Inflammations e.g. IBDs as causes for dysmotility, inflammatory lesions of the Muscularis Propria are common in Crohn’s
- Changes in the connective tissue e.g. absence of the tendinous plexus layer suggesting intestinal desmosis
- Virus ganglionitis, rare cases where virus infections can disturb peristalsis (e.g. Chagas, EBV, Varicella Zoster)
It can also provide information whether the condition is acquired or congenital.
For further information have a look at the publications of Meier-Ruge and Bruder. I won’t go into detail of the biochemical preparations, but if you are interested, have a look at it (imaging, neuroimaging techniques etc)! Even illnesses such as Parkinson can be made visible in changes of the ENS (one of the earliest symptoms are intractable constipation, dysphagia and gastroparesis – even 20 years prior to its diagnosis). Although we know that the ENS is the only independent nervous system, doctors believe that there is some connection in the development of the ENS and central nervous system. Currently, doctors and scientists are also trying to establish some guidelines and classifications of motility disorder and how they manifest in those biopsy findings.
I can recommend the Neurogastroenterology & Motility journal or in Nature Reviews the section on gastroenterology and hepatology. Neurogastro is an active field and its importance is steadily increasing. Unfortunately, there are not that many groups. England and the US seem to be the pioneers. The past years they have also slowly started establishing some guidelines on diagnostics, therapy options and concepts. It is good to see that more GI motility labs are being established in Europe. It seems, however, that those all have their own guidelines, procedures etc which makes it difficult to compare or analyse studies. On the other hand, those patients have quite individual issues and ideally need individual treatment.
Multicentre studies and interdisciplinary research are needed. Gastroenterologists, neurologists, specialists from systematic and autoimmune diseases, visceral surgeons, dietitians, scientists from the mentioned sections and patients have to cooperate. Aside from the typical GI issues, many other co-conditions can arise which need the addition of specialists in hematology, hepatology, visceral surgery, psychology, physiotherapists… Recent studies showed that for functional GI disorders interdisciplinary treatment is far more effective than gastroenterology standard therapy.
I don’t understand why it is so underrepresented. Obviously, there aren’t many patients that suffer from life-limiting or -threatening gastrointestinal issues, but IBS (on which I will elaborate here), for example, is a common condition in our population and in many cases it does decrease the quality of life quite significantly. Further research and cooperation across departments would benefit patients and doctors.
The Iffgd is a good resource to get an overview about conditions, tests, treatment options, research news and events. Via the ESNM you might be able to find clinics and doctors in your area if you are from Europe, via the DGNM and MAGDA in Germany and for Americans there is the ANMS which are the pioneers. In the UK there is the neurogastro and motility section of the BSG and worth mentioning is also the neurogastro group at QMUL. Here are some visual explanations if you are bored of my writing. For more resources have a look here.

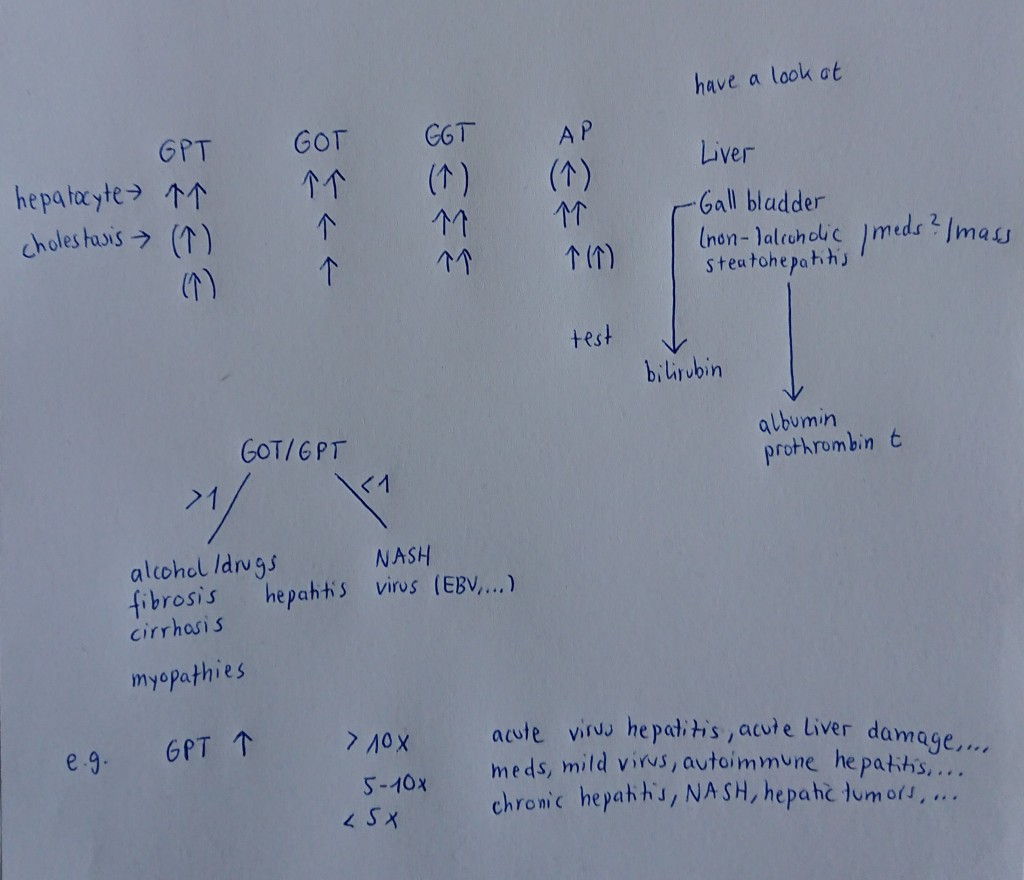
In the last months my liver values have gotten worse and my skin has been turning yellow. Currently, further diagnostics are being done. Obviously, (long-term) parenteral nutrition can cause liver damage, but for me, the doctors think it is due to the colonic atony and small intestine dysmotility.
You might have heard about the enterohepatic circulation, the circulation between liver and the small intestine of metabolic substances or drugs. After the secretion to bile and storing in the gallbladder those get transported to the intestines from where it can get released to the liver again. Intestinal motility and liver function both affect each other. Most of the oral antibiotics, opioids and especially NSAIDS (that’s why you shouldn’t take them often) are all transported in this circulation. When the intestine cannot absorb it due to gut or metabolism changes, it gets stored in the cycle (I believe that this is the reason for the lack of response of my body to most of the meds in the past months). If toxins accumulate in the intestines due to intestinal atony they can be transported via this circulation through the portal vein to the liver as well. Because of the bowel issue, I have developed a non-alcoholic fatty liver (where fat accumulates inside the liver cells) with hepatitis-like liver levels. Steatohepatitis can lead to liver scarring (cirrhosis) and finally liver failure. Typical symptoms are fatigue and upper abdominal pain, later also ascites, jaundice and quite typical are fire-red palms. The liver is very important for digestion, especially of lipids. The liver helps in bile production, stores glucose and vitamins, it supports detoxification and plays an important part in the immune system.
If your liver levels are constantly elevated your doctors should look into it via further blood tests (e.g. lipid levels, hepatitis serology), US of the liver to look for enlargement, duplex US to look for thromboses of the hepatic vessels, if needed additional an MRI or a biopsy. The rule of thumb is to evaluate
- GPT (ALAT)
- GOT (ASAT)
- Gamma GT
- alkaline phosphatate
and if the first two are elevated their relation ASAT/ALAT
- smaller 1: mild liver damage, inflammation (e.g. virus hepatitis)
- greater 1: serious liver damage, necrosis? (e.g. chronic hepatitis, cirrhosis)
If factors such as drugs, meds, alcohol or known preconditions are excluded, one shouldn’t ignore mild elevated values. Patients with sudden abnormally high values should immediately be evaluated. Liver values can point towards hepatic, gall bladder and also cardiovascular problems. They should always be interpreted in context to each other. Also, GPT is a specific hepatic value whereas GOT can also indicate muscle damage.
To support the liver one should cut sugars and rather get calories by eating healthy fats (if you can eat). Here are some liver detox juice recipes.
- 1 beet, ¼ cucumber, ½ apple, juice of 1 lime, some pepper and turmeric, some hemp protein powder
- 1 cup parsley, ½ lemon juice, handful of walnuts, ½ cup papaya, sesame powder
- 1 cup spinach, ½ apple, curmin oil, 1 cup green tea, some ginger, 1 carrot
Following Dr Worm’s Leberfasten (basically degreasing the liver by fasting on a certain protein and veggie diet) and considering that our liver regenerates about 18 times per year, two weeks of some stricter diet is already quite helpful to support this equally important and wonderful organ.

Dysmotility, Dysautonomia, Dysfunctions, Odysseey
Next steps are also a bone mark biopsy (due to the constant low leukocyte number), further evaluation of the dysautonomia symptoms and their relation to the dysmotility and a possible full plexus block. I will explain more about the former in the next posts.
I had a promising call and feedback from doctors that I might benefit from the latter. Reason is that during the first surgery the plexus was partly resected to treat the MALS and as I have already mentioned earlier, the celiac plexus is important for motility. The idea is to completely block it such that the damaged or overreacting/dysbalanced parts cannot forward information to the intestines anymore. Then, the ANS is ‘knocked out’ and the intestines will regulate via the enteral function only (I believe that the sympathetic response dominates in my case). For that to work, however, the ENS has to function (at least a bit) – hence, I am awaiting the pathology results with some worries.
Prior a full CT guided neurolysis (here certain agents like ethanol and lidocaine are applied to the nerve/nerve ganglion in order to cause degeneration of the nerve fibers such that the signals cannot be transmitted anymore) of the ganglion, a multiparametric MRI with nerve imaging and a temporary block is planned. Only if positive (it can also go the other way around and is not without risk), it will be treated by injection.
A plexus block is used to treat intreatable abdominal pain (especially from pancreatic cancer) and as a diagnostic tool e.g. to evaluate whether the patient’s symptoms are from MALS and hence, whether a surgery would improve those symptoms. The doctor will inject a needle into the ganglion from the stomach or back side and the agent will be injected into the plexus.
The celiac plexus is quite deep inside the retroperitoneum, directly above the aorta and in between the other major abdominal vessels such as the SMA and celiac artery. CT guidance of an experienced radiologist/surgeon is necessary to reduce the risk of nearby organ or vessel damage. The patient is also closely monitored afterwards, to evaluate whether the symptoms change, but also intervene if needed. Common reactions (due to the ganglion’s function of the ANS) are hypotony and diarrhea. Risks also include infection due to the puncture, bleeding and lung collapse as well as paraplegia and paralysis (very rare and often caused by temporary ischemia e.g. of the arteria radicularis magna).
If there is the smallest chance that you are reading this and have a background in neurology/neurogastro/interventional radiology (…) or have any experience in the effect of partial resections of the celiac plexus please let me know.
Dysautonomia, also called autonomic dysfunction, is an umbrella term for conditions caused by a dysfunctioning ANS (autonomic nervous system). Patients have problems or even the inability to regulate functions which we normally don’t even think about: digestion and the bladder, heart rate, blood pressure, temperature (which can lead to weird discolourations), sweating, breathing…



Common are:
- POTS: heart rate increase of 30bpm (whilst almost constant blood pressure) or more within the first ten minutes of standing after laying down accompanied with symptoms such as dizziness, fainting, severe tachycardia, sweating, lightheadedness, chest pain… *
- Orthostatic hypotony: low blood pressure dependent on position changes, here blood pressure drop when standing up. This can lead to dizziness, fainting and nausea.
- Autonomic neuropathy: damage of the nerves that transport the ANS signals. The above mentioned functions can all be (separately) affected. It is often part of polyneuropathy which is common in Diabetes patients or occurs after certain meds.
- ….
I will explore more of this topic, causes, diagnostics and treatment options/lifestyle changes and effective exercises to combat those in the next post. Depending on the severity of those conditions the QoL can be significantly reduced or even cause fatal complications.
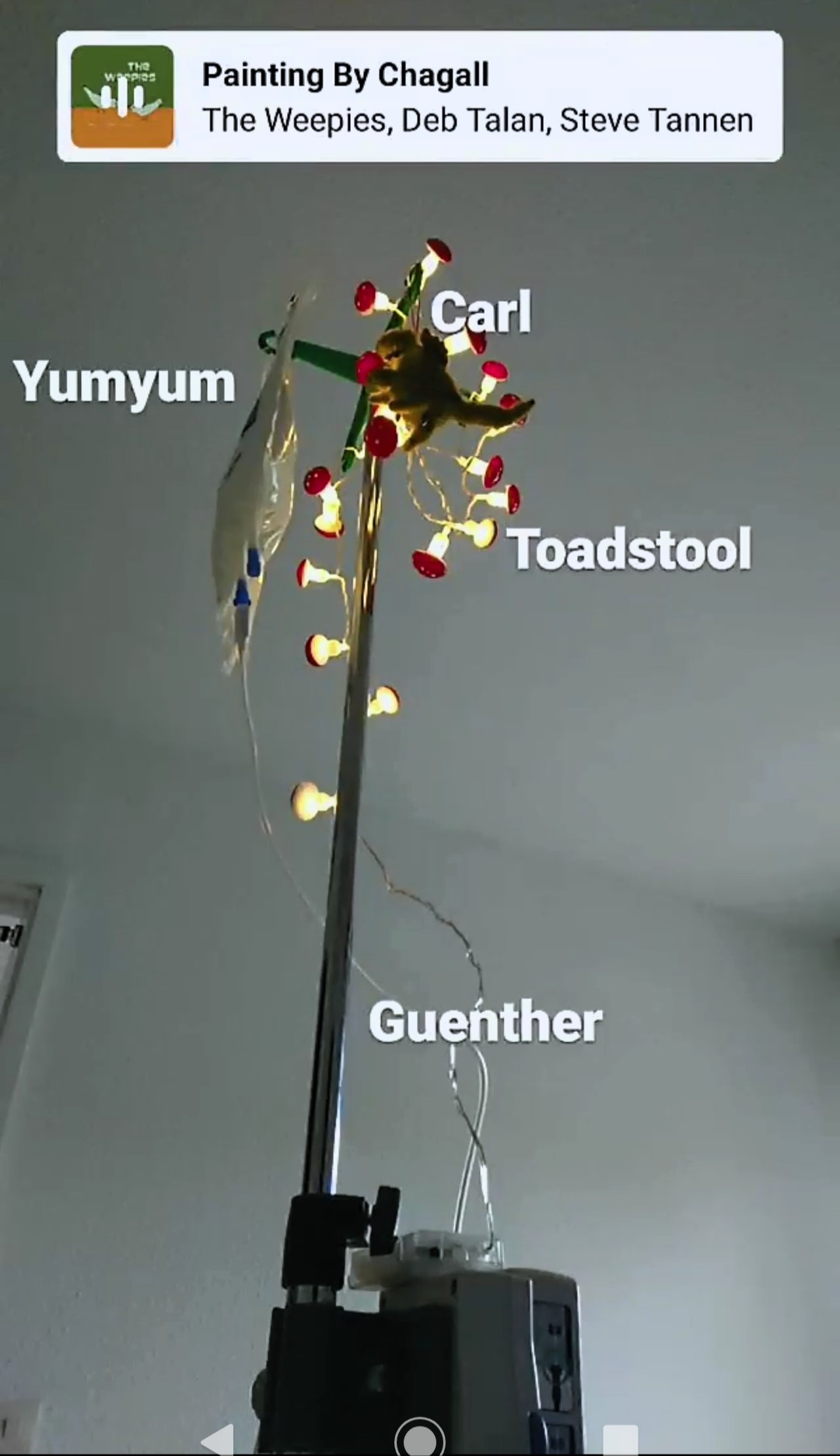
I am very grateful for the possibility of having parenteral nutrition. Back in winter I dropped dangerously low in weight (and I was already quite underweight before that). It took a while to adapt to the new situation, but now Pacman, Günther and Franklin belong to my days just like the pain and the nausea. Next time I will talk about pros and cons of TPN and the risks and complications of cachexia. In the meantime, here are some tips on preparing for the TPN. I am also very happy about the central line as doctors don’t need to waste their hours inserting some iv line (which simply isn’t possible anymore, I can be lucky when blood can be drawn from my foot).
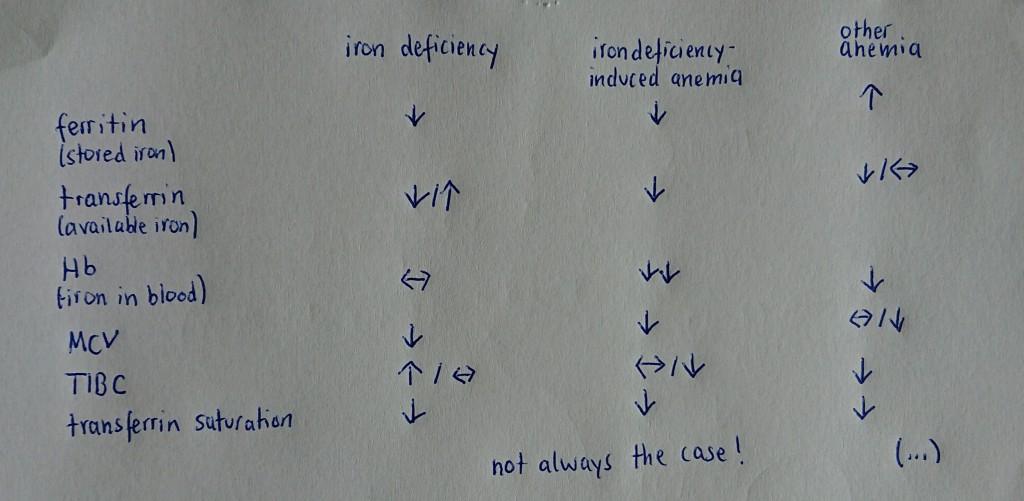
I also received the iron infusion via Pacman which luckily went well and my ferritin storage has increased (a tiny bit). We will probably need to repeat it soon. An iron infusion will be given iv if your iron and ferritin levels are too low. Iron is one of the most important minerals that support blood cell production (hence, oxygen transport in your body i.e. muscle and organ function), hormone production and . Iv iron can be absorbed more readily than oral intake and due to the risk of constipation and the lack of oral absorption in dysmotility patients, they usually get iv infusions. Blood loss, a decreased absorption (GI disorders) or intake of iron (restrictive eating) from your diet as well as an increased need for iron (e.g. during pregnancies) and patients suffering from kidney failure, celiac disease or are on blood thinners can be the cause for iron deficiency which can then further lead to anemia (loss of red blood cells, there are different types, depending on the cause). Typical symptoms are
- (extreme) fatigue, weakness
- tachycardia
- dizziness
- weak immune system, recurrent infections
- always feeling cold, cold feet and hands
- headaches
- breathing difficulties, chest pain
- cognitive difficulties
- unusual cravings (in severe deficiency) like ice, soil …
It is important to check
- serum iron (actual amount of iron in your blood)
- ferritin (how much iron is stored in your body which does indicate an iron deficiency if severely decreased)
- hemoglobin, MCV (average volume of one erythrocyte) and MCH (average Hb amount in one erythrocyte), MCH/MCV = MCHC (average concentration of Hb in the erythrocytes) red blood cell count
- transferrin saturation (how much transferrin is attached to the iron) equivalent to the amount of transferrin
- total iron binding capacity (TIBC) (amount of free transferrin that enables iron transport)
to evaluate whether iron supplement is needed. Usually (not always!), in iron deficient anemia you have low iron, high/normal transferrin (capacity) and low ferritin whereas in anemia of some other issue you have low iron, low/normal transferrin and high or normal ferritin. If your Hb and red blood cells are reduced the iron deficiency is pathological. Low MCV and MCH points towards anemia with small and deficit erythrocytes – probably iron deficiency induced. High MCV and MCH, however, point towards vitamin B/folic acid deficiency induced anemia. (And the list goes on, hematology is very interesting!)
If you suffer from a mild decrease and you are able to eat, you can add more
- tofu
- dark leafy veggies
- liver
- seafood such as tuna (beware endangered species)
- eggs
- wheat
- beans
if tolerated. You can always combine them with some vitamin C e.g. with some orange juice, pepper or tomatoes (or a Kakadu plum or mustard spinach if you get hold of them).
If you take iron supplement pills make sure that you treat iron-induced constipation and don’t take them with milk or other calcium substances. Iron fusions aren’t without risk and should only be given in hospitals such that doctors can intervene if needed. Side effects like GI issues, lightheadedness or muscle/joint pain can occur during or after the infusion, but severe side effects such as breathing problems, severe hypotension or anaphylaxis (tho this is rare, beware if you have MCAS) should be treated immediately. Prior to the infusion I got iv fluids to reduce the risk of severe hypotension. Start with rather small and slow infusions. A hematologist can advise on iron deficiency or anemia problems.

Recommendations, Observations, Motivations
How to survive the apocalypse – songs:
- Sleeping in & We Will Become Silhouettes, The Postal Service
- Noisy Sunday, Patrick Watson
- Fever, Peggy Lee
- Get Me Away From Here, I’m Dying, Belle & Sebastian
- (I’ll Love You) Till the End of the World, Nick Cave and the Bad Seeds
- Hold on, Tom Waits
- Time Zones, Surfaces
- All We Ever Wanted Was Everything, Bauhaus
- Lead me Home, Jamie N Commons
- Grapes of Wrath, Weezers
- Planet Earth, Duran Duran
- When the Smoke Clears, Kina Grannis & Imaginary Future
- For Every Voice That Never Sang, Kishi Bashi
I am not sure how the weather is at yours, but here it has been quite chaotic. Hottest temperatures (that I thought the parenteral nutrition would melt in the hospital), rainy days, pure sunshine, thunderstorms,…
Best songs to listen to during thunderstorms and/or difficult flare-ups:
- At the End Pt 1, Wylder (Into a tangled coral reef where we will never drown/ Now that we’re at the end)
- Fly Like an Eagle, Stereophonics (Did you ever feel like everythings falling/ To fly like an eagle into the dawning/ You know I always feel like skies are falling/ Fly like an eagle and deaths are reborn)
- I Want To Be Well, Sulfjan Steven
- Ride, Amber Run (I’ll be here if you come back home/ Don’t go quietly at night/ Please show some fight)
- After the Storm, Mumford & Sons (Get over your hill and see what you find there/ With grace in your heart and flowers in your hair)
- We Will Become Silhouettes, The Postal Service (And I’m not coming out until this is all over/ And I’m looking through the glass/ Where the light bends at the cracks/ And I’m screaming at the top of my lungs)
- Strangers in the Wind, Cut Copy (Run to the lights of the city/ These moments pass and we’ll be there)
- Care of Cell 44, The Zombies
- Suburban Rain, The Clientele (album)
- Urban Driftwood, Yasmin Williams
- Drift Dive, The Antlers (Slow it down, wait it out/ “We can’t run, but we can go swimming”)
- Duk Koo Kim, Sun Kil Moon
- Great Big Storm, Nate Ruess (Because we’re holding our own in a great big storm/ And though we’re cutting it close, we won’t let go)
I also want to recommend Shoshin Noel music. Despite his struggles he recently published this new song where he ‘poured (his) soul into this track, the ugly, the angry and the honest.’ His honesty and will to fight is inspiring and I wish him all the best.

Book recommendation: Nature Cure
Written by the nature enthusiast Richard Mabey in 2005 this is a book that has been recommended to help in depression. Mabey’s works often cover our relation with nature or the nature-culture relationship. Nature Cure is his personal retreat, he shows how nature helped curing his depression. I enjoyed the accurate descriptions of landscapes and their effect on us. He departs from his old and beloved home to a new one, from deep woods to agriculture landscape, from hills to wide open lands. From the Chilterns to East Anglia to be precise.
In the end it is not the transform of visual nature (but you do learn a lot about the English countryside), but the relation to it and the environment around him that takes him back to life. He uses detailed, honest and quite intense writing (could be too much for some). As a reader you wake up and dream into the poetic and colourful English nature.
‘By a stroke of luck, I was up at dawn on the morning it started. There was a mist hanging over the back meadow, a thin milkiness that was hard to tell from the blowsy lace of the last cow parsley. Then the sun came up and simply parted it, unfolded the life of the new day from the wisps of the night. That, it said, decisively was how it was going to be from now on.’
There are references or descriptions I have never thought about in that particular way, new perspectives, his changing perspective, beautiful words, new words and yet such a familiar rooted theme inside, the former wrapped around it as if you slowly pack out a gift. His observations take us directly into the settings. It motivates us to observe the environment around us, take deep breaths and be aware of the interconnectedness of us and nature. We shouldn’t observe and analyse every part, but be aware of the wonderful details nature provides us and understand us as part of the foam.
Their [cats] effortless passing between the wild and domestic worlds suggests the kind of grace we need as a species to move between nature and culture.
However, there are many sentences one should read a few more times to properly taste them. It is an optimistic story about depression the/a way of healing or recovering (cure is always an optimistic term), but I would suggest it to anyone with mental or physical difficulties. It is also a good book for clinic stays to blend out the lonely, artificial, cold and harsh reality of beeping, doors sliding open and loudly shut, moans and cries in strong, antiseptic and metallic tangs of cold and sterile white-blue hospital rooms.
Mabey starts with John Clare’s ‘The Flitting’, both journeys are equally light.
And still my thoughts like weedlings wild
Grow up to blossom where they can.
from The Flitting, J. Clare


An oriental poppy and noble orchids which Confucius loved so dearly. Thank you for those images and messages. They really encourage us.
Happy belated B-day, Bo!
In June, little Bo turned three (!) years. Unfortunately, I wasn’t able to celebrate with you from the hospitals, but I promise we will go on some exciting adventure soon! I recall the day your father walked towards us so well. It was a magical moment. He would be very proud of you. We are so proud of you.







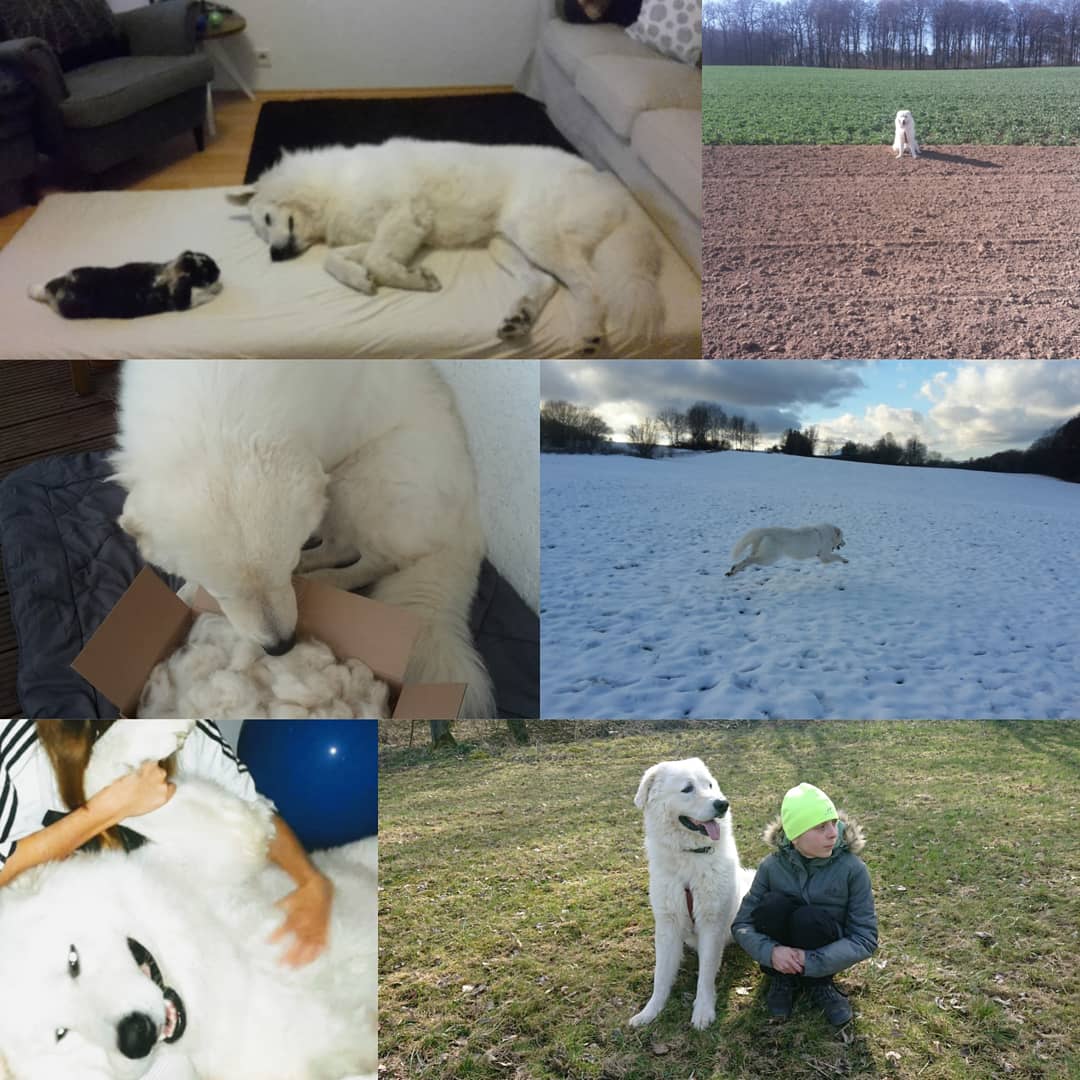



Thank you for always being there.
Thank you for understanding without talking.
Thank you for your calmness.
Thank you for your crazy moves.
Thank you for spreading so much love.
Thank you for your cuddles.
Thank you for your songs.
Thank you for your company.
Thank you for running and exploring, thank you for telling me about your adventures.
Thank you for cheering me up.
Thank you for understanding the pain.
Thank you for sleeping next to me.
Thank you for your love.
Thank you for making us laugh.
Thank you for your wild and funny moments.
Thank you for your acceptance.
Thank you for accompanying me through difficult times.
Thank you for jumping, running and digging.
Thank you for your snoring.
Thank you for your guarding.
Thank you for following your own rules.
Thank you for being a Bo.
A Bo : a unique lovely soul companion
In your eyes I can see the forest, wild, magic, free and full of wonders and possibilities.
I love you so much.
I promise, one day I will show you the best trails to sniff!
And thank you for supporting Argentina (deep down in your heart). Although I don’t stand behind the Copa or Euro, Bo and me are roaring for Argentina and Bo is obviously barking for his home country in the Euro.

*If someone reads this from Germany, where can you get Vitassium by SaltStick or liquidIV from?


That’s a lot of very specific medical knowledge I never knew I’d be interested in reading about lol. Thanks for the update. Wishing you the best despite the bleakness of your situation.
its-running(dot)de appears to have Vitassium in store.
LikeLiked by 1 person
Thank you very much!
LikeLike